
Exclusive Care EPO
Exclusive Provider Organization
Summary Plan Document
January 2022
EPO: 2022
2
TABLE OF CONTENTS
INTRODUCTION ..................................................................................................................... 5
SECTION 1: ELIGIBILITY AND ENROLLMENT .................................................................... 7
Health Plan Eligibility ............................................................................................................ 7
Dependent Eligibility ............................................................................................................. 7
Continued Coverage for Disabled Dependents if your employer group provides dependent
coverage .............................................................................................................................. 8
Plan Enrollment Identification Card ...................................................................................... 8
Mid-Year Changes ............................................................................................................... 8
Termination of Benefits and Re-Enrollment .......................................................................... 9
Reinstatement .................................................................................................................... 10
Keeping Enrollment Information Up-to-Date ....................................................................... 10
Cost of Enrollment in the Plan ............................................................................................ 10
SECTION 2: HOW THE EPO PLAN WORKS ...................................................................... 11
Choice of Providers ............................................................................................................ 11
Changing Primary Care Providers ...................................................................................... 12
Scheduling Appointments ................................................................................................... 12
Referrals to Specialists ....................................................................................................... 13
Second Medical Opinion .................................................................................................... 13
SECTION 3: EPO PLAN BENEFITS .................................................................................... 14
Schedule of Benefits .......................................................................................................... 14
SECTION 4: EXPLANATION OF COVERED SERVICES ................................................... 18
Inpatient Services ............................................................................................................... 18
Emergency Care/Urgent Care/Urgently Needed Services ................................................. 19
Outpatient Services ............................................................................................................ 20
Other Services.................................................................................................................... 22
SECTION 5: PLAN EXCLUSIONS AND LIMITATIONS ...................................................... 23
General Exclusions ............................................................................................................ 23
Specific Exclusions ............................................................................................................. 24
EPO: 2022
3
Limitations .......................................................................................................................... 29
SECTION 6: OUTPATIENT PRESCRIPTION DRUG PROGRAM ....................................... 30
How The Program Works .................................................................................................. 30
The Drug Formulary ........................................................................................................... 30
Pre-Authorization of Non-Formulary Drugs ........................................................................ 31
Maintenance Drug Dispensing ........................................................................................... 31
Mandatory Generic Substitution ......................................................................................... 32
Mail Order Service .............................................................................................................. 32
Exclusions and Limitations ................................................................................................. 33
Dispensing Quantity Limitations ......................................................................................... 34
SECTION 7: MENTAL HEALTH/SUBSTANCE ABUSE SERVICES ................................... 34
Covered Services ............................................................................................................... 34
What To Do In Emergencies .............................................................................................. 35
Exclusions And Limitations ................................................................................................. 35
SECTION 8: CHIROPRACTIC CARE BENEFIT .................................................................. 37
How The Chiropractic Care Benefit Works ......................................................................... 37
Covered Services ............................................................................................................... 37
Exclusions And Limitations ................................................................................................. 37
SECTION 9: OUT-OF-AREA COVERAGE FOR QUALIFIED DEPENDENTS .................... 38
How the Out-of-Area Coverage Works ............................................................................... 38
Choice of Providers ............................................................................................................ 38
Second Medical Opinion .................................................................................................... 38
SECTION 10: PLAN GENERAL PROVISIONS ................................................................... 43
Claim Payment Procedures ................................................................................................ 43
Member Grievence Procedure ........................................................................................... 44
COBRA Continuation of Coverage ..................................................................................... 51
Health Insurance Portablility and Accountability Act (HIPAA) ............................................ 54
SECTION 11: PAYMENT BY THIRD PARTIES ................................................................... 59
SECTION 12: HEALTH PLAN ADMINISTRATION AND INTERPRETATION ..................... 61
SECTION 13: DEFINITION OF TERMS ............................................................................... 62

EPO: 2022
4
Alternative formats of this publication can be made available upon request. Please contact
Member Services at (800) 962-1133
EPO: 2022
5
INTRODUCTION
The Exclusive Care Exclusive Provider Organization (EPO) is a Health Plan provided for
employees and under age 65 retirees of the County of Riverside, their Eligible Dependent(s) and
for the employees and dependents of other Qualified Public Employer Groups.
Exclusive Care provides comprehensive health care services through a Network of Participating
Hospitals, Medical Groups and Physicians. This Network is called an Exclusive Provider
Organization (EPO). The Plan’s Benefits include preventative care and services, specialty
services, hospitalization and prescription drugs, with only a low Copay required from you. You
must receive all your services through the Network for Benefits to be paid (except in certain
emergencies, described in this Summary Plan Document). Members of Exclusive Care will
receive an identification card that must be presented each time a Member receives services.
This plan does provide an Out-of-Area Schedule Of Benefits under Exclusive Care’s Out-of-Area
coverage for your eligible qualified dependents living outside the EPO Plan Service Area. The
qualified dependent may receive treatment and services and seek reimbursement through the
Plan according to the Member Coinsurance and limitations indicated in the Summary Plan
Document. Plan Benefits are paid according to the reimbursements and limitations shown in
the “Out-of-Area Schedule of Benefits” section.
This Summary Plan Document (SPD) provides a description of how the Plan works and an
explanation of what is and is not covered. The SPD is the primary governing document for all
Plan coverage decisions and will be the basis for final determination for the provision of Benefits.
It is the Plan’s intent to comply with all laws and regulations that are applicable, regardless of
whether they are specifically described in this SPD.
Beginning in 2014, the Affordable Care Act requires most people of have health care coverage
that qualifies as “minimum essential coverage”. This plan meets or exceeds the requirements
for minimum essential coverage.
In addition, the Affordable Care Act establishes a minimum standard of benefits for a health plan.
The plan must pay a minimum of 60% of the cost of benefits. This plan meets or exceeds the
requirements for minimum value standard.
The County of Riverside is pleased to provide this Exclusive Care EPO Health Plan for you and
your Eligible Dependent(s). If you have any questions about Benefits provided by the Plan, a
Representative is available to assist you at the Member Services Department phone number
listed below.
EPO: 2022
6
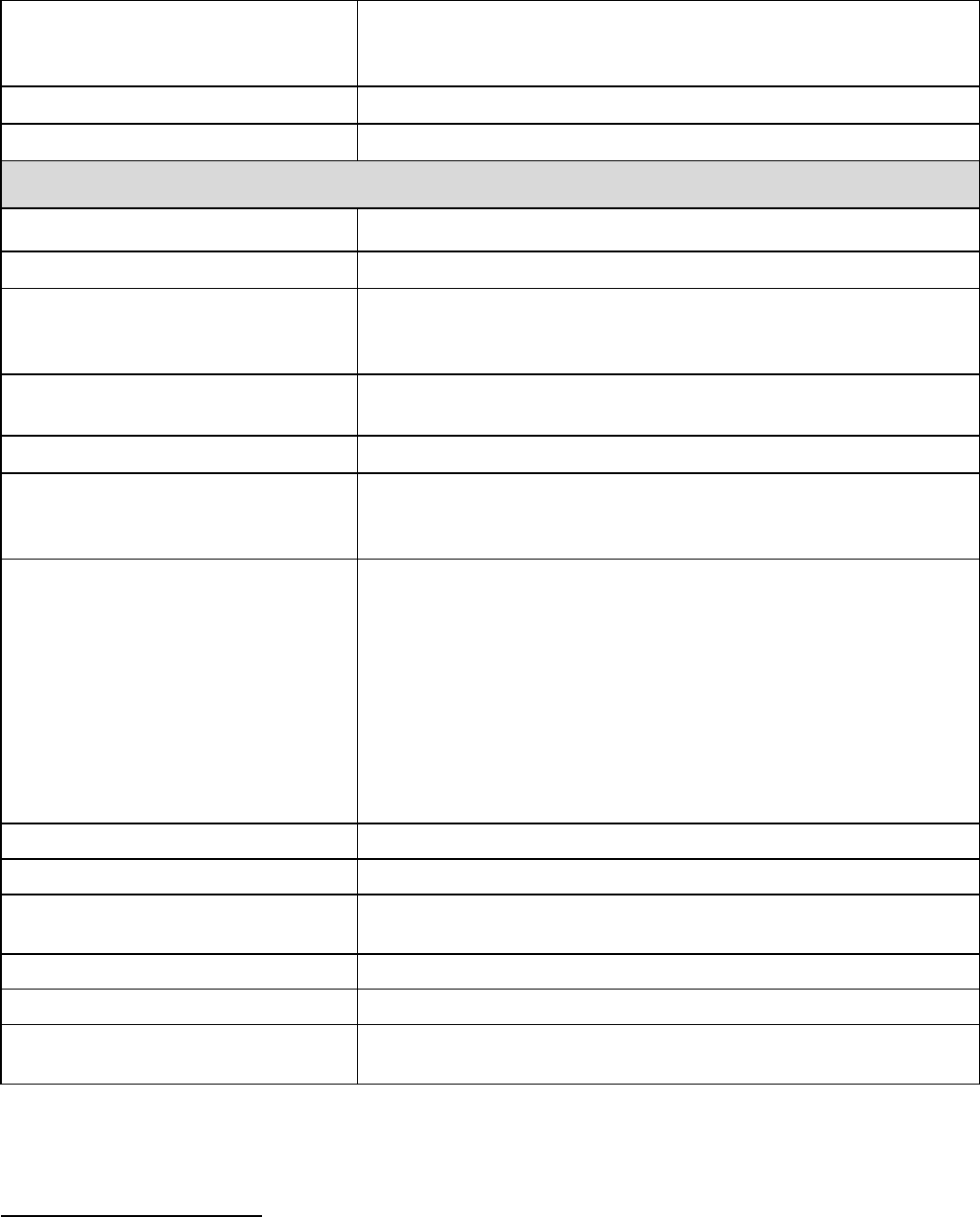
Exclusive Care EPO
Plan Sponsor
The County of Riverside and any other Qualified Public
Employer Group for its own Members
Plan Administrator
Assistant CEO, Director of Human Resources
County of Riverside, Human Resources
4080 Lemon Street, 7
th
Floor
Riverside, CA 92502
(951) 955-3510
Plan Mailing
Address
Exclusive Care
P.O. Box 1508
Riverside, CA 92502-1508
www.exclusivecare.com
Member Services
(800) 962-1133
Monday through Friday
8:00 a.m. - 5:00 p.m. Pacific Coast Time
Type of Plan
The Plan is a welfare benefit plan established and
operated by the County of Riverside that provides health
care Benefits for eligible M
embers of participating
Qualified Public Employer Groups.
Type of Funding
The Plan is self-insured and unfunded. In other words, the
Plan is funded through premium contributions that are
made by its Members and participating Qualified Public
Employer Groups, and Benefits are paid from Plan assets
which are maintained by the County of Riverside. The
Plan Administrator may also establish a trust for the
payment of Benefits.
Plan Year
The Plan year begins on January 1 and ends on December
31. The Plan’s financial records are based on the Plan’s
fiscal year.
Plan Establishment
The Plan was established for the exclusive benefit of its
Members in 1999.
SPD Effective Date
The effective date of this SPD is January 1, 2022
The Plan Administrator reserves the right to change, modify or terminate, in whole or in part, this
Plan at any time.
EPO: 2022
7
SECTION 1: ELIGIBILITY AND ENROLLMENT
Health Plan Eligibility
You are eligible to enroll in the EPO Health Plan if:
• you are an employee or Eligible Dependent of the County of Riverside or of a Qualified
Public Employer Group that offers the Exclusive Care EPO Plan, and you reside or
work in the Exclusive Care EPO Plan Service Area;
• you are a County of Riverside retiree under age 65.
You are eligible for the Out-of-Area Schedule Of Benefits if:
• you are a qualified, Eligible Dependent of a County of Riverside employee or
Qualified Public Employer Group employee living outside the EPO Plan Service
Area
Eligibility requirements are established by your employer group and are detailed in the Group
Healthcare Services Agreement signed by your employer group. Contact your employer group
for the dependent eligibility requirements including any age limits for dependents. County of
Riverside eligibility requirements are detailed in employee benefits medical plan eligibility
requirements available through Human Resources.
Dependent Eligibility
If your employer group provides dependent coverage and you are enrolled in the Health Plan
option applicable to you, your legal spouse or Domestic Partner and Eligible Child (ren) may
also enroll in the same Health Plan, subject to the following:
• Domestic Partners must sign, agree, and meet the requirements specified in the
Employers Declaration of Domestic Partnership and a signed Statement of Financial
Liability to the satisfaction of the County of Riverside or the Qualified Public Employer
Group;
• Your children, or those of your legal spouse or Domestic Partner, who are under the
employer group’s limiting age may enroll in the same Health Plan if they meet one of the
eligibility requirements as set forth below:
i) They must be natural born children, or children placed for the purposes of foster
care or adoption or legally adopted children; or
ii) They must be children for whom you, or your legal spouse or Domestic Partner are
appointed a legal guardian by a court; or
iii) They must be children for whom you or your legal spouse or Domestic Partner are
required to provide health coverage pursuant to a qualified medical child support
order (“QMCSO”) or who reside with you (generally in the absence of the natural
or adoptive parent) and who are economically dependent upon you; or
iv) They must be children that reside with you, generally in the absence of the natural
or adoptive parent; for whom you have legal custody or guardianship. A copy of
the court-ordered custody must be on file.
EPO: 2022
8
Dependent enrollment and eligibility shall not be denied because the dependent:
• Was born to a single person or unmarried couple; or
• Is not claimed as a dependent on your federal income tax return.
Continued Coverage for Disabled Dependents if your employer group provides
dependent coverage
Children who are over your employer group’s limiting age, who reside with either you or your
separated or divorced spouse, are incapable of self-sustaining employment by reason of mental
handicap, debilitating Chronic Condition, or physical handicap that existed continuously prior to
your employer group’s limiting age and who are dependent upon you for support and
maintenance, and who would otherwise be eligible to enroll as Eligible Children except for the
fact that they are older than the limiting age, may enroll or continue enrollment beyond the
limiting age, provided proof of such incapacity is provided within sixty (60) days of the onset of
the Disability, or attainment of the limiting age.
The Plan may require ongoing proof of the dependent’s incapacity and dependency, but not
more frequently than annually following the first two years following the attainment of the limiting
age or the onset of the Disability. Such proof shall include a written statement by a licensed
psychologist, psychiatrist, or other Physician to the effect that such dependent is incapable of
self-sustaining employment by reason of mental handicap, debilitating Chronic Condition, or
physical handicap.
Plan Enrollment Identification Card
Once you are enrolled in the Plan, you and any enrolled dependent(s) will receive a new
Member packet with identification cards, identifying you as a Member of the Exclusive Care
Plan. Carry your identification card with you at all times. Present your identification card
whenever you receive services.
Mid-Year Changes
Enrollment changes that are permitted during a Calendar Year are called qualified status
changes and include:
• Marriage;
• Divorce or legal separation;
• Birth or adoption of a child;
• Death of an Eligible Dependent;
• Change in an Eligible Spouse’s employment that would affect medical coverage or a
significant change in an Eligible Spouse’s employer-offered medical coverage;
• Loss of a dependent’s eligibility under another plan; or
• Entitlement to Medicare.

EPO: 2022
9
You must notify your employer group within the timeframe established by your employer
group from the date of the qualified status change; usually thirty (30) days.
Coverage designation may be changed during the Calendar Year for any of the qualified status
changes listed above. Failure to notify your employer group in a timely manner may result in the
inability to correct and/or refund premium payments. Documentation that substantiates the
qualified change must accompany the paperwork required by your employer group. Coverage
for mid-year changes becomes effective the first day of the month following the date you notify
your employer group of the status change; however, newborns or newly adopted dependents
are covered as of the date of their birth or adoption contingent upon the timely completion of the
enrollment paperwork.
If you wish to change your election based on a qualified status change, you must establish that
the change is on account of and corresponds with the qualified status change. The employer
group shall determine whether a requested change is on account of and corresponds with a
qualified status change. As a general rule, a desired election change will be found to be
consistent with a qualified status change event if the event affects coverage eligibility. In addition,
you must also satisfy the following specific requirements in order to alter your election based on
that qualified status change:
• Loss of Dependent Eligibility: If your Eligible Spouse or Eligible Dependent Child(ren)
lose coverage for any of the following reasons, you may only cancel coverage for the
affected dependent:
i. Your divorce, annulment or legal separation from your Eligible Spouse; or
ii. The death of your Eligible Spouse or your Eligible Dependent; or
iii. Your dependent ceases to satisfy the eligibility requirements for coverage.
For example, if your Eligible Child reaches the limiting age and no longer meets the Plan’s
eligibility requirements, you may cancel that child’s coverage mid-year, but you may not cancel
your Eligible Spouse’s coverage too.
• Gain of Coverage Eligibility Under Another Employer’s Plan: If you, your spouse, or
your dependent child becomes eligible for coverage under another employer’s plan (or
qualified benefit plan) as a result of a change in your marital status or a change in your
spouse’s or your dependent child’s employment status, your election to cancel or
decrease coverage for that individual under the Plan would correspond with that qualified
status change only if coverage for that individual becomes effective or is increased under
the other employer’s plan.
Termination of Benefits and Re-Enrollment
A Member’s coverage may be terminated if the Member:
• becomes deceased;
• ceases to be eligible for coverage based on the employer group’s rules of eligibility;
• voluntarily cancels coverage;
• becomes Medicare eligible as a result of age or Disability;
EPO: 2022
10
• fails to pay the required premium;
• was never eligible for membership;
• engages in fraud or deception;
• permits misuse of identification card;
• fails to cooperate with Exclusive Care’s Third Party Lien and Non Duplication of Benefits
Rights;
• has his/her coverage terminated at the request of the employer group;
• engages in an act of gross misconduct, which causes the interruption of the normal
operations of the Plan.
Plan coverage and eligibility for Benefits stop on the date coverage ends. Any Member who is
hospitalized when his/her enrollment terminates for any reason other than the voluntary
termination of coverage shall be granted a continuation of Benefits with respect to medical
conditions that were present or preexisting at the time of hospitalization or occurred during the
hospitalization and which require continued hospitalization. This continued coverage should not
extend beyond the 91st day following the termination.
If for any reason the Plan terminates your coverage, the effective date of the coverage
termination will be the date determined by the Plan.
Reinstatement
A Member may be reinstated at the discretion of Exclusive Care under the following
circumstances:
i. At the request of your employer group (along with payment of premiums).
ii. Payment of premium in arrears by you.
The maximum retroactive reinstatement period is 60 days.
Keeping Enrollment Information Up-to-Date
The Plan maintains enrollment information in order to communicate with you. Please help by
keeping this information up-to-date. If there are any changes in your name, marital status,
address, or phone number, please contact your employer group so your records may be updated
and the updated information forwarded to the Plan. Most importantly, the Plan requires up-
to-date information in the event your coverage ends, in order to send COBRA
continuation of coverage information as well as your “Prior Credible Coverage”
certificates to the correct address, and to any dependents that may not be living at the
same address.
Cost of Enrollment in the Plan
You are responsible for the payment of the entire premium for health care coverage for yourself
and your enrolled dependents. It is your responsibility to stay informed about your payroll
premium deductions and your benefit elections. If you have questions about these, contact your
employer’s human resources, payroll or designated department.
EPO: 2022
11
SECTION 2: HOW THE EPO PLAN WORKS
The Plan provides Covered Services to Plan Members with virtually no paperwork. To obtain
services, contact your Primary Care Provider (PCP), schedule an appointment, and show your
Member identification card. If additional care or specialty services are needed, your Primary
Care Provider will coordinate with Exclusive Care for approval, authorization and claim
processing.
Choice of Providers
PLEASE READ THE FOLLOWING INFORMATION SO YOU WILL KNOW THOSE
PROVIDERS (OR GROUP OF PROVIDERS) THROUGH WHICH YOU MAY OBTAIN HEALTH
CARE SERVICES. IT IS YOUR RESPONSIBILITY TO KNOW WHERE TO OBTAIN
SERVICES. THIS WILL ENSURE THAT NO OUT-OF-POCKET EXPENSES WILL BE
INCURRED BY YOU.
A unique feature of the Plan is your ability to choose a private practice Physician who practices
in your community, a County of Riverside-employed Physician at Riverside County Regional
Medical Center, or a County of Riverside Public Health Clinic, as your Primary Care Provider
(PCP). You may choose whichever PCP you prefer from the provider Network. The provider you
choose can be convenient to your home or workplace. Our Member Services staff can assist
you with finding your nearest PCP.
To be covered, services must be provided by Exclusive Care Physicians, Hospitals, Specialists
or other medical facilities assigned to you (except in the case of life-threatening emergency
services).
All Exclusive Care providers are listed in the Exclusive Care provider directory. You select a
PCP from the provider directory, and this provider coordinates all your health care services. You
may obtain a copy of the provider directory by contacting Exclusive Care’s Member Services
Department, or by accessing the Plan’s website at www.exclusivecare.com.
When selecting your PCP:
• The PCP you choose must be a Participating Provider and within a 30-mile radius of your
primary residence or workplace;
• You and your Eligible Dependents may each choose a different PCP;
• The name of the PCP you choose must be indicated using the provider ID number listed
in the directory on your Benefit Election Form/Enrollment Form;
• If you do not select a PCP at the time of your enrollment, one will be selected for you.
Please refer to the “Changing Primary Care Provider” section of this document for detailed
information about changing your provider after your initial enrollment;
• Your PCP will be listed on your identification card. Always present your card wherever
you attend appointments or receive treatment.

EPO: 2022
12
The Plan contracts with Medical Groups and individual Physicians to provide primary care
services to Members, and with Hospitals to provide hospitalization services. These Participating
Medical Groups, Physicians and Hospitals, in turn, may employ or contract with individual
Physicians.
The Plan’s Participating Hospitals are paid on a discounted fee-for-service or fixed charge basis
for Covered Services. Most acute care, sub-acute care, transitional Inpatient care and Skilled
Nursing Facilities are paid on a fixed charge basis for each day of Inpatient care.
Changing Primary Care Providers
You may change your Primary Care Provider (PCP) by calling the Member Services Department
at (800) 962-1133, ext 1. Your change will be effective the same business day.
Requests for a change of Primary Care Provider may be denied if:
• The Plan determines the transfer would have an adverse effect on the quality of care
given to you;
• The requested provider is closed to new patients.
The Plan may require that you select a new Primary Care Provider if there is a breakdown in
resolving conflicts between you and your existing Primary Care Provider. In this event, you will
be required to select a new Primary Care Provider within thirty-one (31) days of receiving notice
from the Plan. If it is determined by the Plan’s Medical Management Unit that a provider change
would adversely impact your medical care, the Plan will make every effort to enable you to
continue your relationship with your current Primary Care Provider wherever possible.
IT IS IMPORTANT TO KNOW WHEN YOU ENROLL IN THE EPO PLAN THAT SERVICES ARE
PROVIDED THROUGH THE PLAN’S DELIVERY SYSTEM OF PARTICIPATING PROVIDERS
AND FACILITIES. THE CONTINUED PARTICIPATION OF ANY INDIVIDUAL PHYSICIAN,
HOSPITAL, OR OTHER PROVIDER CANNOT BE GUARANTEED.
Scheduling Appointments
Once you have selected your PCP, appointments are simply a phone call away. For routine
office visits, call for an appointment at least 48 hours in advance. For preventative care
appointments, such as a periodic health evaluation, or a well woman care visit, call at least four
weeks in advance. These appointments are scheduled based on availability.
If you need more immediate attention, call your PCP and request the next available appointment.
If your PCP is unavailable, please refer to your provider directory or contact the Member Services
Department for assistance locating contracted urgent care facilities. If you use a non-Network
urgent care facility, the services may not be covered by the Plan and you will be responsible for
the Billed Charges.
If you need to cancel an appointment, please contact your PCP as soon as possible.
EPO: 2022
13
Referrals to Specialists
Your PCP will coordinate all of your health care needs. If your PCP determines that you need to
see a Specialist, he/she will request an appropriate Specialist referral on your behalf by
contacting the Plan’s Medical Management Unit. A member of this unit’s staff will contact your
PCP with the outcome of the request. You will also receive notification from the Plan of approval
for a Specialist appointment, along with the address and phone number for scheduling your
appointment, and any other necessary instructions.
The Specialist is usually pre-authorized to treat you for a specific number of visits for a given
condition, but may request additional visits or diagnostic studies if needed.
IMPORTANT: Prior authorization is not required for many services, and your PCP may
make a direct referral to a contracted provider. Annual well woman exams, OB/GYN
consultations and office visits, mammograms, bone mineral density testing, initial
chiropractic evaluation, mental health services, family planning, and several other
services may be referred directly by your PCP without prior authorization. The direct
referral form and a list of services covered under the direct referral policy may be viewed
at:
http://www.exclusivecare.com/Portals/19/DirectReferralrev052316.pdf?ver=2016-05-23-
1355757-327
A referral request may also be reviewed by the Plan’s Physician Review Committee. The
Physician Review Committee meets on a regular basis, depending on the volume of special
requests or care issues, and authorization or referral requests that require review. Decisions
may be made by the Medical Management Unit and/or Exclusive Care’s Medical Director,
outside of a formal committee meeting to assure a timely response to emergency or urgent
requests.
Second Medical Opinion
You, or your treating PCP, may request a second medical opinion by submitting a referral
request in writing to the Medical Management Unit. The Medical Management Unit will provide
you with a list of Specialists from which you and your PCP may choose a provider for your
second medical opinion. The Plan reserves the right to submit any request to the Medical
Director or Physician Review Committee for review. Non-covered treatments or conditions are
subject to the “Member Grievance Procedure” (described later in this SPD) and will not be
reviewed by the committee.
Second medical opinions can only be rendered by a Physician qualified to review and treat the
medical condition in question. “Out-of-Network” referrals will be approved only when the services
requested are not available within the EPO Network. If a second medical opinion is deemed to
be not Medically Necessary and the request is denied, you may appeal the denial by following
the procedures outlined in the “Member Grievance Procedure” section of this SPD. For more
information, please contact the Member Services Department.

EPO: 2022
14
SECTION 3: EPO PLAN BENEFITS
Schedule of Benefits
As a Member of the Plan, you should coordinate all your health care services through your
Primary Care Provider (PCP). The Schedule of Benefits below summarizes the services that
are covered, the amount the Plan will pay, and your Copay amounts.
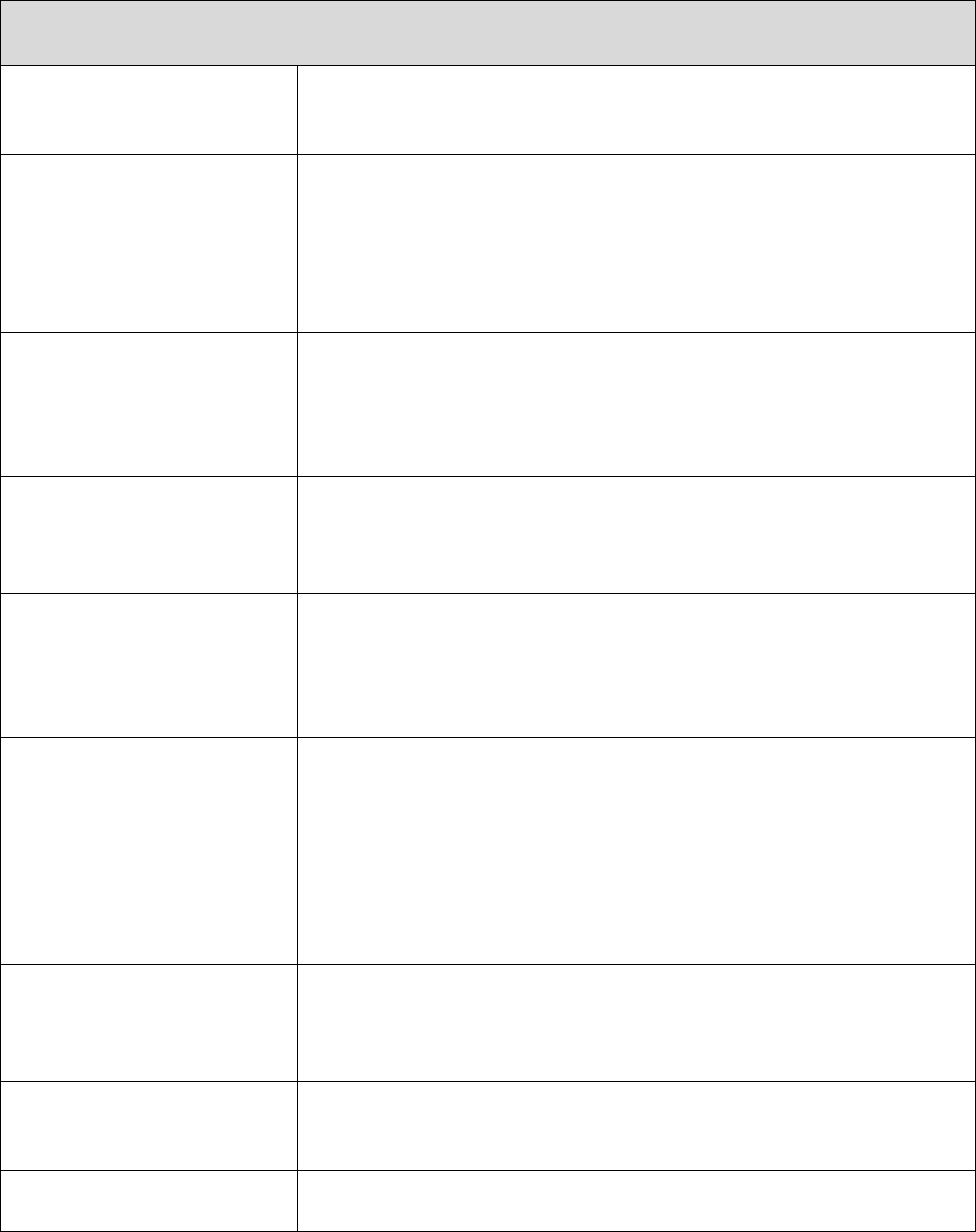
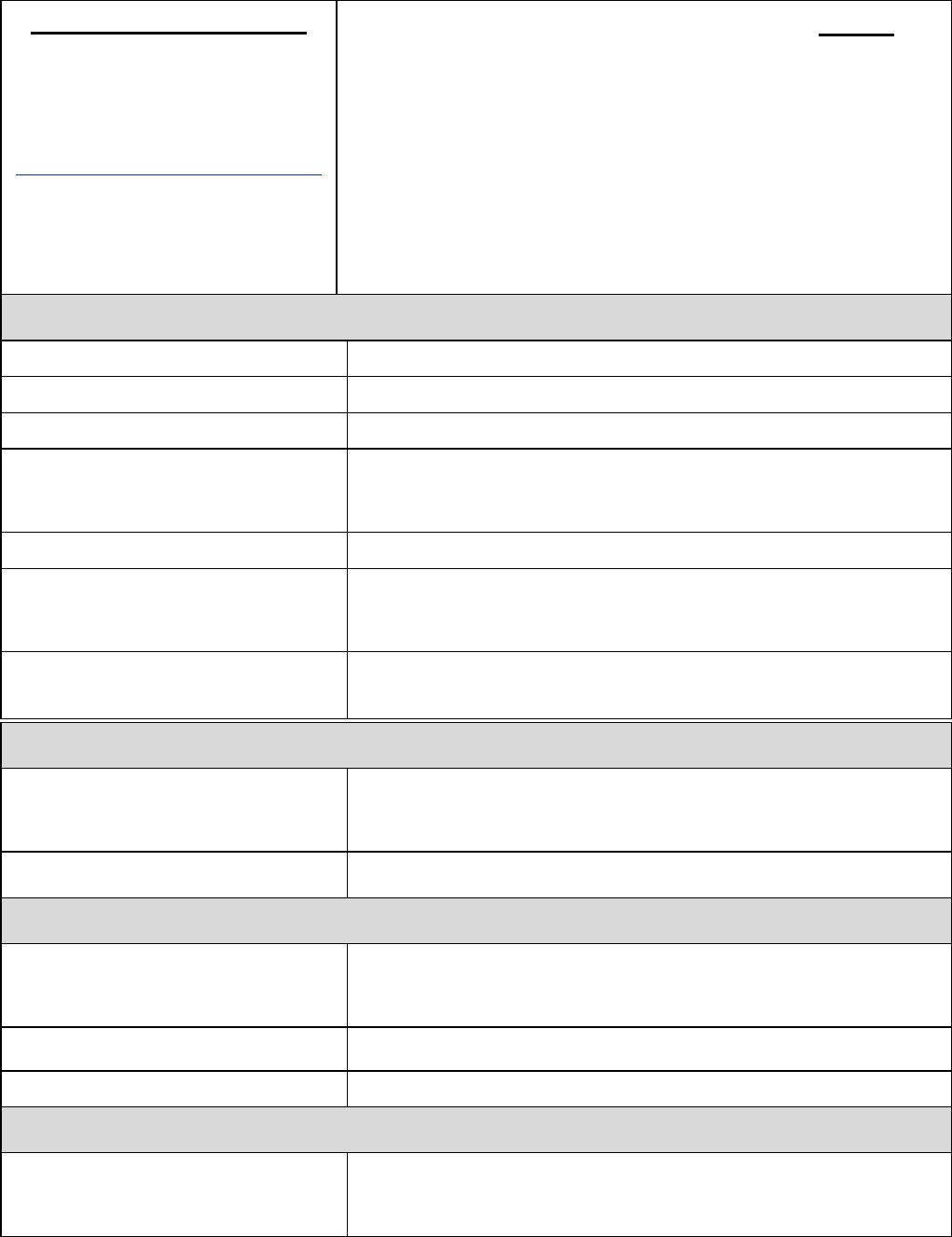
Schedule of Benefits – EPO Plan
Choice of Physician Any Participating Primary Care Physician
Deductible – Individual None
Deductible – Family None
Out-of-Pocket Maximum $1,500/Member, maximum $3,000/Family per Calendar Year
Lifetime Maximum Benefit Unlimited
Pre-existing Condition Fully Covered
Outpatient/Office Visits
Coverage Level
Physician Office Visits 100% after $15 Copay
Hospital Clinic Visits 100% after $15 Copay
Immunizations 100%
Maternity Care 100%
Periodic Health Evaluations 100%
Diagnostic X-ray & Lab
100%
Well Baby Care 100%
Well Woman Care 100%
Vision Exams (screening and
refraction)
100%, 1 Vision Exam per Calendar Year
Outpatient Prescription Drugs
• Prescription Drug Coverage is administered by the Plan’s Pharmacy Benefit Manager (PBM)
•
Pharmacy Benefit Manager (PBM): Navitus Health Solutions. Up to 90 Days
Navitus
www.navitus.com
Phone: (866) 333-2757
FORMULARY DRUGS
1-34 days
35-90 days
Tier 1; Generic Drugs
$10 Copay
$20 Copay
Tier 2; Preferred Brand Name
Drugs
$25 Copay $50 Copay
Tier 3; Non-Preferred Brand Name
Drugs
$50 Copay $100 Copay
Significant or new therapeutic class drugs: 50% copay. Some formulary
and all non-formulary drugs require pre-authorization.
Members with Diabetes and Members who use Antihyperlipidemic and
Antihypertensive drugs have no copays for Tier 1 and Tier 2 Supplies
and Medication.
EPO: 2022
15
RUHS
- Mail Order Service
Medical Center Retail Pharmacy
26520 Cactus Ave.
Moreno Valley, Ca 92555
Phone (951) 486-4515, option 5
www.ruhealth.org/services/pharmacy
(mail order prescriptions only)
FORMULARY DRUGS
90 days
Tier 1; Generic Drugs
$20 Copay
Tier 2; Preferred Brand Name Drugs
$50 Copay
Tier 3; Non-Preferred Brand Name Drugs
$100 Copay
Significant or new therapeutic class drugs: 50% copay. Some formulary
and all non-formulary drugs require pre-authorization.
Members with Diabetes and Members who use Antihyperlipidemic and
Antihypertensive drugs have no copays for Tier 1 and Tier 2 Supplies
and Medication.
Hospital & Emergency Room
Ambulance 100%
Ambulatory Surgical Center 100% at Network facility only
Physician Hospital Visits 100%
Inpatient Hospital Services
$100 per admission at Network or non-Network facilities; non-
Network facility coverage for emergency only (services subject to
medical review)
Outpatient Hospital Services 100% at Network facility only; non-Network facilities not covered
Hospital Emergency Room (Copay
waived if admitted)
100% after $100 Copay at Network or Non-Network facilities; non-
Network facility coverage for emergency only (services subject to
medical review)
Urgent Care/Urgently Needed
Services
100% after $20 Copay at Network or non-network facility.
(services subject to medical review)
Severe Mental Health Treatment
Inpatient Care
$100 per admission at Network or non-Network facilities; non-
Network facility coverage for emergency only (services subject to
medical review)
Outpatient Care 100% after $15 Copay
Non-Severe Mental Health Treatment
Inpatient Care $100 per admission at Network or non-Network facilities; non-
Network facility coverage for emergency only (services subject to
medical review)
Outpatient Care - Individual 100% after $15 Copay
Outpatient Care - Group 100% after $15 Copay
Substance Abuse Treatment
Inpatient Care
$100 per admission at Network or non-Network facilities; non-
Network facility coverage for emergency only (services subject to
medical review)
EPO: 2022
16
Inpatient Detoxification
$100 per admission at Network or non-Network facilities; non-
Network facility coverage for emergency only (services subject to
medical review)
Outpatient Hospital Services 100% at Network facility only
Outpatient Office Visit 100% after $15 Copay
Other Benefits
Allergy Testing & Treatment 100% after $15 Copay
Chiropractic Care 100% after $15 Copay; benefits limited to 12 visits/Calendar Year
Members Requiring Diabetes Care
Pharmacy Copays are waived for all Generic and Preferred Brand
Name injectable and oral antidiabetic medications and diabetic
supplies (testing strips, syringes, etc.)
Members taking Antihyperlipidemic
and Antihypertensive Drugs
Pharmacy Copays are waived for all Generic and Preferred Brand
Name antihyperlipidemic and antihypertensive
drugs
Durable Medical Equipment 50% Copay (services subject to medical review)
Other Medical Equipment (As
defined in Section 4: Outpatient
Services)
100%
Family Planning
Elective Pregnancy Termination
Infertility Services
Tubal Ligation
Vasectomy
100% after $50 Copay for 1
st
trimester; $100 Copay for 2
nd
trimester; (3
rd
trimester only covered if pregnancy life threatening to
mother)
50% Copay; up to a maximum of $10,000 lifetime benefit (services
subject to medical review)
100%
100%
Home Health Care 100%
Hospice Care 100%
Physical Therapy 100% after $15 Copay up to 30 visits/Disability within a 90-day
period
Skilled Nursing Facility
$100 per admission up to 100 days/Disability
Hearing Aid Instrument $3,000/Member; once every 36 months
Bariatric Surgery $100 per admission at Network facility only (services subject to
medical review)
An explanation of terms used in this Schedule of Benefits follows below, to help you get
the most out of your coverage:
Pre-Existing Conditions
EPO: 2022
17
The Plan has no pre-existing conditions limitation. Therefore, there are no limitations, waiting
periods or exclusions for being treated for any diagnosis or condition currently on record for you
or your enrolled dependents as long as services are Covered Services.
Medically Necessary
The Plan only covers Medically Necessary health care services. See Section 13 - Definition of
Terms, for a more detailed explanation. Certain services provided by non-Network facilities
require a medical review by the Plan’s Medical Management Unit, to establish whether or not
the services were Medically Necessary.
Copay
These are the amounts that you pay for certain Covered Services. For office visits, prescription
drugs and other basic services, you are required to pay a dollar amount at the time you receive
services (e.g. $15 Copay for an office visit). After you pay this Copay, the Plan pays for Covered
Expenses up to the Allowed Charge, subject to all other terms and limitations described in the
Schedule of Benefits, General Provisions, or Exclusions and Limitations sections of this SPD.
For Inpatient services and some Copays you pay that are a percentage of the cost, you normally
pay your share after the provider bills the Plan and the Plan has paid its portion of the covered
costs.
Deductible – Individual/Family
The Deductible is the portion of the cost of medical expenses you must pay each Calendar Year
before the Plan will pay any Benefits. There are no individual or family Deductibles required
with the Exclusive Care EPO Plan.
Out-of-Pocket Maximum
The Plan helps protect you from costly medical expenses by limiting the total amount you pay
out of your own pocket for certain services in any one Calendar Year. When the amount that
you or any enrolled dependent has paid for these services reaches the designated level (the
Out-of-Pocket Maximum), that covered member will pay nothing further for Covered Services for
the rest of the Calendar Year (up to any benefit maximums that may apply). Out-of-Pocket
amounts you pay which do not count towards each Member’s Out-of-Pocket Maximum include:
• Deductibles (in the case of the EPO Plan, there are no Deductibles);
• Charges in excess of the Allowed Charges covered by the Plan;
• Charges for services that are not covered by the Plan, such as a charge for a service
listed as an exclusion;
• Charges for services for which no benefit is payable because the dollar or benefit limit
has been exceeded;
Lifetime Maximum Benefit
Unlimited

EPO: 2022
18
SECTION 4: EXPLANATION OF COVERED SERVICES
The Plan reserves the right to review all claims submitted for payment to verify the validity of
services based on Medical Necessity. Emergencies are subject to Medical Necessity review,
and all Members of the EPO admitted to a non-Network facility will be transferred to a Network
facility when medically stabilized.
The Plan covers preventative, certain wellness services, and other Medically Necessary health
care services and supplies provided to you. Covered Services include:
Inpatient Services
Room and Board
Semi-private room, intensive care unit (private room), operating, recovery and special treatment
rooms
Additional Inpatient Services
Laboratory services, X-rays, drugs, anesthesia, medications and biologicals. All other Medically
Necessary Inpatient services such as Physical, Speech, Occupational and Respiratory Therapy,
hemodialysis and administration of blood and blood plasma, including the collection and storage
of autologous blood, nursing care and Durable Medical Equipment;
Physician, Surgeon and Anesthesiologist Services
Skilled Nursing Facility or Convalescent Care
Administration of Blood and Blood Plasma
The processing and storage of autologous blood for scheduled medical procedures;
Maternity Care
Hospital and other related services, Physician and medical services for normal vaginal delivery,
Caesarean Section, and complications of pregnancy. Elective termination of pregnancy
coverage is limited to first and second trimester; no coverage during the third trimester unless
mother’s life is in jeopardy.
The Plan will not restrict Benefits for any Hospital length of stay in connection with childbirth for
the mother or eligible newborn child to less than forty-eight (48) hours following a normal vaginal
delivery, or less than ninety-six (96) hours following a Caesarean Section, or require that a
provider obtain authorization from the Plan for prescribing a length of stay not in excess of the
above periods. However, Federal law generally does not prohibit the mother’s or newborn’s
attending provider, after consulting with the mother, from discharging the mother or the newborn
earlier than 48 hours (or 96 hours as applicable). In any case, the Plan may not, under Federal
law, require that a provider obtain authorization from the Plan for prescribing a length of stay not
in excess of 48 hours (or 96 hours);

EPO: 2022
19
Newborn Care
If your employer group provides spousal dependent coverage, newborns who are born while the
mother is covered under the Plan are also covered by the Plan for up to 30 days after birth.
These newborns will be identified using the mother’s Member ID. Newborn dependent coverage
will only be extended beyond the first 30 days after birth if the child is enrolled in the Plan as a
dependent within the first 60 days after birth.
Breast Reconstructive Surgery
Coverage will be provided to a Member who is receiving Benefits for a Medically Necessary
mastectomy and who elects breast reconstruction after mastectomy for:
Reconstruction of the breast on which a mastectomy has been performed;
Surgery and reconstruction of the other breast to produce a symmetrical appearance;
Prostheses; and treatment of physical conditions of all stages of mastectomy, including
lymphedemas;
This coverage will be provided in consultation with the attending Physician and the patient, and
will be subject to the same Deductibles, Copays, and maximums, if any, that apply to the
mastectomy;
Inpatient Dental Care
Inpatient services associated with dental procedures under the following circumstances:
the Member is a child, up to 6 years old, with a dental condition (such as baby bottle
syndrome) that requires administration of general anesthesia in a hospital setting for
dental repairs of significant complexity (e.g., multiple amalgam and/or resin-based
composite restorations, pulpal therapy, extractions or any combinations of these noted
or other dental procedures); or,
the Member exhibits physical, intellectual, or medically compromising conditions, is in
need of dental treatment that requires administration of general anesthesia and for
whom administration of a general anesthesia can only be safely performed in a hospital
setting. Conditions include but are not limited to: mental retardation, cerebral palsy,
epilepsy, cardiac problems and hyperactivity (verified by appropriate medical
documentation).
Limited to Inpatient Hospital and anesthesiologist charges; charges for the actual dental
procedure performed by a dentist or an oral surgeon are not covered.
Emergency Care/Urgent Care/Urgently Needed Services
Ambulance Service
Land or air;
Emergency Care Services

EPO: 2022
20
Emergency Care Services are medical, emergency room or Hospital services required as the
result of a medical condition, manifesting itself by the sudden onset of sufficient severity, which
may include severe pain, such that a reasonable person would expect the absence of immediate
medical attention to result in:
Placing your health in serious jeopardy;
Serious impairment to bodily functions; or
Serious dysfunction of any bodily organ or part;
Examples of emergencies include heart attacks, strokes, poisonings, and sudden inability to
breathe;
Urgent Care/Urgently Needed Services
Urgent Care or Urgently Needed Services are Medically Necessary services required after
regular business hours to prevent serious deterioration of your health resulting from unforeseen
illness or injury manifesting itself by acute symptoms of sufficient severity which may include
severe pain, such that the treatment cannot be delayed until your Primary Care Provider is
available;
Urgent Care or Urgently Needed Services are provided for less serious medical conditions than
Emergency Care Services, such as:
Non life-threatening cuts which nevertheless require immediate suturing to ensure proper
healing;
Acute illnesses where a delay in care would result in a serious deterioration in your health;
Follow-Up Care
If you require additional services following Emergency Care or Urgent Care/Urgently Needed
Services, you must obtain these services from your Primary Care Provider. If additional services
or a referral to a Specialist is necessary, your Primary Care Provider can make this request on
your behalf. Follow-up care provided in an emergency room is not a covered expense;
Non-Qualifying Services (EPO Plan ONLY)
Medical or Hospital services which do not qualify as Emergency Care or Urgent Care/Urgently
Needed Services received from non-Participating Providers are not covered by the Plan. For
example, medical care provided outside the Plan’s Service Area will not be covered if the need
for care is for a known or Chronic Condition that is not manifesting itself by acute symptoms as
defined Emergency Care or Urgent Care/Urgently Needed Services section;
Outpatient Services
PCP Office Visits
Periodic Health Evaluations (gender-specific, age-specific), Well Baby Care and Well Woman
Care visits;
EPO: 2022
21
Specialist and Consultant Visits
Home Health Care Visits
Prenatal and Postnatal Care
Allergy Testing and Treatment
Hearing Screening when performed in a Physician’s office.
Ambulatory Surgical Center
Diagnostic X-Ray and Laboratory Services
Procedures consistent with established medical practices.
Durable Medical Equipment
Rental (but not to exceed the purchase price) or purchase of Durable Medical Equipment used
in your home.
Other Medical Equipment
Corrective appliances, artificial aids, Prosthetics and Orthotics that are part of a corrective
appliance; therapeutic footwear (limits may apply);
Urinary catheters (covered for a Member who has permanent urinary incontinence or
permanent urinary retention).
Physical and Occupational Therapy limited to treatment only where short-term therapy is
expected to result in a near-term significant improvement.
Charges for Second Medical Opinion
Immunizations
Childhood immunizations, Hepatitis B and certain adult immunizations when Medically
Necessary or when required for employee safety in the workplace.
Hearing Aid Benefit
To access your hearing aid benefit, first consult your Primary Care Provider who will determine
if an evaluation is needed and will submit the referral request on your behalf. Once authorized,
you may schedule an appointment with an audiologist. Covered Expenses include:
An audiological evaluation to measure the extent of hearing loss;
Hearing aid evaluation to determine the most appropriate make and model of hearing aid;
Limited to once every thirty-six (36) months for the hearing aid instrument (monaural or
binaural), ear mold(s), the initial battery, cords and other ancillary equipment, or
maintenance and repair of current hearing aid device. Includes visits for fitting,

EPO: 2022
22
counseling, adjustments, and repairs at no charge for a one-year period following the
provision of a covered hearing aid.
You may be asked to pay the full cost of the hearing aid at the time of purchase. Should this
occur, you can receive prompt reimbursement (up to any benefit limitations that apply) by
submitting a copy of the provider’s bill and your receipt to the Plan’s Claims Department.
Family Planning Services
Infertility testing and treatment - procedures consistent with established medical practices
in the treatment of Infertility when authorized through your Primary Care Provider, but
limited to diagnosis, diagnostic tests, medication and surgery;
Physician visits for contraceptive devices and oral contraceptive prescriptions;
Vasectomy;
Tubal ligation;
Injectable contraceptives;
Implantable contraceptives.
Well Woman Care
Annual pelvic examination and PAP smear based on current recommendations from the
US Preventive Services Task Force and your PCP’s assessment of need (subject to
medical review);
Periodic clinical breast examination and annual clinical breast examination for women
age 40 and above; and,
Baseline mammogram for women of average risk starting at age 40, and annually
thereafter. Mammograms may be performed earlier if clinically indicated.
Other Services
Hospice Care
Hospice Care services are covered up to the benefit level described in the Schedule of Benefits
if the Member:
Has been certified by the attending Physician to have 180 days of life expectancy or less;
Decided to no longer pursue aggressive medical treatment; and,
The goal of treatment is to provide supportive nursing care and counseling to the Member
during the terminal phase of illness, social services evaluation, and Home Health aid services.
Organ Transplants
Cost of organ procurement - when the organ is harvested from a living donor, the Plan will cover
Medical and Hospital services and other costs of a donor or prospective donor when the recipient
is a Member:

EPO: 2022
23
Medical expenses incurred by the organ donor for the surgical procedure and
associated Hospital stay for harvesting of the donated organ if expenses incurred
exceed any benefits available through any other insurance plan. Expenses are limited to
the donor’s Inpatient Hospital stay for the organ harvesting, and related follow-up care
for sixty (60) days following the organ harvesting.
Costs related to a donor search - limited to a maximum benefit of $15,000 for each
organ transplant when the search is conducted by a special transplant facility, or $5,000
for each organ transplant when the search is conducted by other facilities.
Travel expenses - limited to a maximum lifetime benefit of $7,000 for organ transplants
performed at a special transplant facility, or $3,000 for organ transplants performed at
other facilities. Travel expenses associated with an organ transplant are covered if the
facility at which the transplant is performed is more than 100 ground miles from the
organ recipient’s home address. Child care or charges for house-sitting are not covered
by the Plan. Benefits paid will be based on actual incurred costs. Covered travel
expenses include:
• Coach airfare on a public airline for the organ recipient and one companion (two
companions if the organ recipient is a minor child) to travel to and from the site of
the transplant. A “companion” includes the organ recipient’s legal spouse, legal
parent(s) or legal guardian(s);
• Reimbursement for mileage at the federal maximum rate for use of a personal
car or rental car used to travel to and from the site of the transplant;
• Up to $200/day for reasonable and necessary lodging and meals for the organ
recipient (while not confined) and companion(s). The $200/day maximum applies
to the organ recipient and companion(s) collectively, not individually.
Bariatric, Gastric Bypass and other Weight Reduction Surgeries
For additional Plan Exclusions and Limitations, refer to Weight Control Programs section.
SECTION 5: PLAN EXCLUSIONS AND LIMITATIONS
General Exclusions
All services not specifically included in the preceding “Schedule of Benefits” and “Explanation Of
Covered Services” sections of this document;
Any services requiring approval and authorization by the Plan and/or your Primary Care Provider
where pre-authorization was not obtained (except for Emergency Care or Urgent Care/Urgently
Needed Services);
All services prior to your effective date of coverage or subsequent to your coverage termination
date;
If you are a Member of the EPO Plan, Services rendered by non-Participating Providers where
you have refused treatment available, or where authorized by the Plan and/or your Primary Care
Provider within the Plan Service Area;

EPO: 2022
24
Services received that, based on Medical Management review, are not Medically Necessary, in
accordance with professionally recognized standards of proven and effective medical practice
recognized within the organized medical community;
Services which are part of a plan of treatment for a Non-Covered Service. This may include
services and supplies to treat medical conditions which are recognized by the organized medical
community in the State of California, in conformance with professionally recognized standards
of practice, to be direct and predictable consequences of such non-Covered Services; Medically
Necessary services required to treat medical conditions that may arise but are not predictable in
advance, such as unexpected complications of surgery are not subject to this exclusion;
Charges incurred while on active duty with the Army, Navy or Air Force of any country or
international organization;
Charges submitted for which the Member is not obligated to pay, or for which the Member would
not have been billed had insurance coverage not existed.
Specific Exclusions
Acupuncture, Acupressure, Biofeedback
Ambulance Service (except when Medically Necessary or necessitated by a life-threatening
emergency)
Bone Marrow Transplants (when Experimental or Investigational)
Cosmetic Surgery
Services or supplies related to cosmetic surgery, unless required as a result of an illness
or injury sustained while covered under the Plan, or to correct a functional defect resulting
from a congenital abnormality or developmental anomaly;
Complications of cosmetic surgery or drugs prescribed for cosmetic purposes;
Surgery to alter and improve your physical appearance or to improve your self-esteem,
which provides no improvement to a functional impairment;
Custodial Or Domiciliary Care
Homemaker services, Respite Care, convalescent care or extended care not requiring skilled
nursing;
Dental Care, Dental Appliances
All services required for prevention and treatment of diseases and disorders of the teeth,
including, but not limited to:
Oral exams, X-rays, routine fluoride treatment, plaque removal, tooth decay, dental
embryonal tissue disorders, periodontal disease;
EPO: 2022
25
Anesthesia, repair and restoration, tooth extraction, replacement of missing teeth, dental
implants, dentures and other oral prosthetic devices;
Dental services rendered more than six months after an accidental injury to sound natural
teeth;
Treatment, prevention or relief of pain for dysfunction of the temporomandibular joint or
the muscles of mastication;
Disabilities Connected To Military Services
Treatment for disabilities connected to military service for which you are legally entitled through
a Federal government agency, and to which you have reasonable access;
Durable Medical Equipment, Corrective Appliances, Prosthetics:
Replacement of lost Durable Medical Equipment, corrective appliances, or prosthetics;
Additional optional accessories to Durable Medical Equipment, corrective appliances, or
prosthetics, which are primarily for your comfort or convenience;
Personal comfort items such as electric heating or cooling units, orthopedic mattresses
or support chairs, blood pressure instruments, scales, elastic bandages or stockings,
waterbeds, exercise equipment and swimming pools including home and car remodeling
or modification. This includes prosthetics that require surgical connection to nerves,
muscles or other tissues (bionic) and prosthetics that have electric motors to enhance
motion (myoelectronic);
Emergency Care Services - Non-Network Facility
If you are enrolled in the EPO, Emergency Care services are covered in a non-Network facility
only as long as a life-threatening condition exists, and a transfer to a Network facility would be
medically inappropriate. Routine follow-up care, including treatments, procedures, X-rays, lab
work, Physician visits, Rehabilitation, and skilled nursing care will not be authorized once it is
determined by the Plan that it is medically reasonable for you to obtain these services from a
Participating Provider. Members should contact the Plan within twenty-four (24) hours of
receiving treatment in the event of an Emergency Care situation. Failure to do so may result in
a reduction or denial of Benefits;
Experimental Or Investigational Treatment
Unless otherwise dictated by Federal or state law, decisions as to whether a particular treatment
is Experimental or Investigational, and therefore not a covered Benefit, are determined by the
Plan’s Medical Director or his/her designee, based upon criteria established pursuant to the
following guidelines:
• Any drug, device, treatment, or procedure shall be deemed as Experimental or
Investigational treatment if, as determined solely by the Plan, any one or more of the
following criteria are met:
It cannot be lawfully marketed without the approval of the United States Food and
Drug Administration (“FDA”) and such approval has not been granted at the time of its
use or proposed use;
EPO: 2022
26
It is the subject of a current investigational new-drug or new-device application on file
with the FDA;
It is being provided pursuant to a written protocol that describes among its objectives
determinations of safety and/or efficacy as compared with the standard means of
treatment;
It is being delivered or should be delivered subject to the approval and supervision of
an institutional review board as required and defined by Federal regulations and other
official actions and publications issued by the FDA and the HHS;
The predominant opinion among experts as expressed in the published authoritative
literature is that usage should be substantially confined to research settings;
The predominant opinion among experts as expressed in the published authoritative
literature is that further research is necessary in order to define safety, toxicity,
effectiveness or effectiveness compared with conventional alternatives;
It is not investigational or experimental in itself pursuant to the above, and would not
be Medically Necessary, but for the provision of a drug, device, treatment, or
procedure which is Investigational or Experimental.
• The exclusive sources of information to be relied upon by the Plan in determining whether
a particular treatment is Experimental or Investigational, and therefore not a Covered
Service under the Plan, are limited to the following:
The Member’s medical records;
The protocol(s) pursuant to which the drug, device, treatment, or procedure is to be
delivered;
Any consent document the Member, or his/her representative, has executed or will be
asked to execute, in order to receive the drug, device, treatment, or procedure;
The published authoritative medical or scientific literature regarding the drug, device,
treatment, or procedure at issue as applied to the medical condition at issue;
Opinions of other agency/review organizations e.g., ECRU Health Technology
Assessment Information Service, HAYES New Technology Summaries or AHCPR
(Agency for Health Care Policy and Research);
Expert medical opinion; and
Regulations and other official actions and publications issued by the FDA and HHS.
A terminally ill Member may be entitled to an expedited hearing in cases in which a proposed
treatment is denied as Experimental or Investigational (refer to the “Member Grievance
Procedure” section of this SPD for more information);
Eye Surgery
Surgery to correct refractive error, such as, but not limited to radial keratotomy, refractive
keratoplasty;
Foot Care
EPO: 2022
27
Routine foot care, such as removal or reduction of corns and calluses, clipping of toenails,
treatment for flat feet, fallen arches, and chronic foot strain, except as determined to be Medically
Necessary;
Genetic Testing
If not related to a specific medical diagnosis for a covered Member;
Institutional Services And Supplies - Non-Eligible
Any services or supplies furnished by a non-eligible institution, which is defined as other than a
legally operated Hospital, Ambulatory Surgical Center, or Medicare-approved Skilled Nursing
Facility, or which is primarily a place of rest, a place for the aged, a nursing home, or any similar
institution, regardless of how denominated;
Non-Licensed Professionals
Treatment for any illness or injury when not attended by a licensed Physician, surgeon or other
licensed Health Care Professional;
Nursing - Private Duty
Unless determined to be Medically Necessary and ordered by your Primary Care Provider and
approved by the Plan’s Medical Director;
Nutritional Supplement Formulas
Phenylketonuria (PKU) formula is limited to under age thirteen (13), or as Medically Necessary;
Organ Donor Services
Medical and Hospital services and other costs of a donor or prospective donor when the recipient
is not a Member of the Plan;
Organ Transplants
Organ transplants that are not Medically Necessary and organ transplants considered
Experimental or Investigational as defined herein;
Outpatient Prescription Drugs
The “Outpatient Prescription Drug Program” section of this SPD describes how Outpatient
prescription drugs are covered by the Plan;
Out-Of-Area Emergency Care services
For EPO Plan Members, coverage is limited to the Benefits outlined in the “Emergency Care
and Urgently Needed Services” section of this document. The Member will be responsible for
the bill if services are obtained out-of-area and are not determined to be a life-threatening
emergency.
Physical Examinations
Routine physical examinations for insurance, licensing, employment, school, camp, recreational
or organizational, including appearances at hearings or court proceedings, examinations
EPO: 2022
28
precedent to engaging in travel, or other non-preventative purposes, pre-employment physicals
or vocational Rehabilitation, or for pre-marital and pre-adoption purposes;
Pregnancy Of Covered Dependent
Services related to a non-spousal dependent’s pregnancy are limited to prenatal care/normal
delivery of the covered dependent. Charges for all services provided to the newborn, incurred
after the birth/delivery of the dependent’s newborn are excluded, including pediatric services;
Private Rooms And Comfort Items
Personal or comfort items and private rooms during Inpatient hospitalization, unless Medically
Necessary, such as cable television, telephones, communication devices, exercise equipment,
air purifiers, humidifiers, saunas, hot tubs, therapeutic mattresses, and supplies or any other
similar devices or appliances;
Public Facility Care
Care of conditions for which state or local law requires treatment in a public facility (however,
the Plan will reimburse you for out-of-pocket expenses incurred by you for any Covered Services
delivered at such public facility);
Injuries or illnesses sustained while incarcerated in a municipal, state or Federal prison;
Emergency Care and Urgent Care/Urgently Needed Services required after participating in a
criminal act (covered only until the Member is stabilized and placed on a police hold);
Notwithstanding the foregoing, in compliance with California Health & Safety Code section
1374.12, nothing in this provision shall be deemed to restrict the liability of the Plan with respect
to Covered Services solely because such services were provided while the Member was in a
state Hospital;
Random Drug Testing
All drug testing for a non-medical diagnosis regardless if court ordered;
Recreational, Educational, Hypnotic Therapy
All treatment and related diagnostic testing, except as provided as part of an otherwise covered
Inpatient hospitalization);
Rehabilitation
Long term, maintenance, or chronic- level Rehabilitation services such as Physical,
Occupational and Speech Therapy provided on an Inpatient or Outpatient basis;
Reversal of Voluntary Sterilization
Sexual Dysfunction
Treatment for sexual dysfunctions or inadequacies unless pre-authorized by the Plan;
Skilled Nursing Care/Transitional Care

EPO: 2022
29
Skilled Nursing Facility room and board charges incurred beyond the limits outlined in the
“Schedule of Benefits” section for each qualifying condition. A qualifying condition is a medical
condition which requires skilled nursing services, which as a practical matter, determined by the
Plan and the Member’s Primary Care Provider, cannot be delivered in a setting other than a
Hospital or a Skilled Nursing Facility. A medical condition will not be considered a qualifying
condition if during the 60 days preceding the medical condition, the Member has received skilled
nursing services.
Social Disorders
Services which are primarily oriented towards treating a social, educational or learning disorder,
rather than a medical diagnosis, including treatment for dyslexia, and behavioral modification
therapy;
Surrogate Pregnancy
Third-Party Liability Services
Please refer to the “Payment by Third Parties” section of this document;
Vision Care
Eye refractive examination, corrective lenses and frames, contact lenses, contact lens fitting and
measurements (except post cataract extraction, keratoconus, aphakic or corneal bandages);
Weight Control Programs (Inpatient or Outpatient)
Eating disorder programs for dietary control, or other treatment of obesity such as food and
proprietary food supplements, vitamins and laboratory tests in association with weight reduction
programs. The Plan does cover certain Medically Necessary Bariatric Surgery procedures
ordered by your Primary Care Provider and approved by the Plan’s Medical Director.
Work-Related Illnesses/Injuries
Injury, sickness or disease which arises out of or in the course of any employment, or which is
covered under any workers’ compensation law or similar law.
Limitations
Circumstances Beyond Control
If, due to circumstances not reasonably within the control of the Plan, such as complete or partial
destruction of facilities, war, riot, civil insurrection, or similar causes, the provision of Covered
Services is delayed or rendered impractical, neither the Plan nor its Participating Providers have
any liability or obligation for such delay or failure to provide services;
Major Disaster Or Epidemic
In the event of any major disaster or epidemic, Participating Providers shall provide or attempt
to arrange for the provision of Covered Services insofar as is practical, according to their best
judgment, within the limitations of such facilities and personnel as are then available, but neither
EPO: 2022
30
the Plan, nor its Participating Providers have any liability or obligations for delay or failure to
provide any such services or personnel if such lack is the result of such disaster or epidemic.
SECTION 6: OUTPATIENT PRESCRIPTION DRUG PROGRAM
Refer to this section of this Summary Plan Document for details of how all Outpatient prescribed
and non-prescribed medications are covered.
The Plan provides Benefits for Outpatient prescription drugs on the Navitus (The Plan’s
Pharmacy Benefit Manager) Formulary (“Drug Formulary” or “Formulary”), when prescribed by
a Participating Physician or licensed dentist, or a non-Participating Physician in certain
emergency situations, or for a Member with Out-of-Area coverage.
How The Program Works
• Present your prescription and Navitus identification card at any Participating Pharmacy;
• Pay your Copay for each 30-day supply of prescription drugs you have filled, or the retail
cost of the prescription, whichever is less.
• Receive your medications.
The Drug Formulary
The Drug Formulary is a list of Outpatient prescription drugs that will be covered by the Plan
without preauthorization when a prescription is filled at a Participating Pharmacy. The Formulary
is created and regularly updated by a Pharmacy and Therapeutic Committee that consists of
practicing Physicians and pharmacists. The Formulary is revised periodically to incorporate new
developments in pharmaceutical care. A limited number of formulary drugs require pre-
authorization.
The evaluation of the products included in the Formulary is a continuous process resulting in the
review of new and existing medications to ensure the Formulary is up-to-date and meets the
needs of Members and their providers.
The Formulary is extensive and covers all therapeutic classes of drugs, including medications
that treat both Acute and Chronic Conditions. Acute Conditions include, but are not limited to,
the flu, colds and other short-term illnesses. Chronic Conditions include, but are not limited to,
glaucoma, diabetes, high blood pressure, heart disease, and asthma. The Formulary includes:
• Federal Legend Drugs: Any medicinal substance which bears the legend: “Caution:
Federal law prohibits dispensing without a prescription”;
• State Restricted Drugs: Any medicinal substance that may be dispensed by prescription
only according to state law;
• Compounded Medication: Any medicinal substance that has at least one ingredient that
is Federal Legend or State Restricted in a therapeutic amount;

EPO: 2022
31
• Generic Drugs: Generic Drugs will be automatically substituted for Brand- Name Drugs if
available, unless the Physician has indicated “Dispense as Written” on the prescription;
• Insulin, insulin syringes, blood glucose test strips, lancets, inhaler extender devices,
epipens and anakits;
• Federal Legend oral contraceptives, prescription diaphragms.
If you would like additional information about the Formulary, contact Navitus Customer Care at
(866) 333-2757.
Pre-Authorization of Non-Formulary Drugs
If a non-Formulary drug is prescribed, it will not be covered unless the non-Formulary drug is
pre authorized. All pre authorization requests for non-Formulary drug treatments may be initiated
by your Physician. Non-Formulary drugs that are not otherwise excluded from coverage will be
authorized in the following instances:
• No Formulary alternative is appropriate and the Plan determines the drug is Medically
Necessary for your individual needs;
• The Formulary alternative has failed after therapeutic trial. Your prescribing Physician
will be asked to provide a copy of your medical chart notes that specifically state treatment
failure with the Formulary drug;
• You have been under treatment and remain stable on a non-Formulary prescription drug
and conversion to a Formulary drug would be medically inappropriate;
• You have experienced a typical allergic reaction or medically established adverse
reaction which are effects related to the chemical properties of the Formulary drug. These
allergies and/or adverse effects are attributed to formulations or differences in absorption,
distribution or elimination; and,
• Your Physician provides evidence in the form of documents, records or clinical tests,
which demonstrate that use of the requested non-Formulary drug over the Formulary drug
is Medically Necessary, as determined by the Plan.
Authorizations for non-Formulary medications will be given for a time period varying from six
months to indefinitely, upon request for the prescribed medication.
Note: The Plan reserves the right to expand the pre authorization requirement for any drug
product to assure adherence to FDA-approved indications and national practice standards. The
Formulary has medications added and deleted throughout the year based on the
recommendations of the Pharmacy and Therapeutic Committee’s quarterly review.
Maintenance Drug Dispensing
Maintenance drugs will be dispensed for up to a 90-day supply through Navitus Participating
Pharmacies, or mail order service. These products include, but are not limited to:
• Antiarthritics
• Antiasthmatics

EPO: 2022
32
• Anti-clotting drugs
• Antiepileptic drugs
• Antihypertensives
• Anti-Parkinson drugs
• Birth control pills
• Cardiac drugs
• Cholesterol and lipid lowering agents
• Diuretics
• Gastrointestinals
• Glucose test strips
• Hormones
• Insulin and Insulin syringes
• Oral contraceptives
• Oral hypoglycemics
• Prenatal vitamins
• Psychotropics
• Thyroid suppressants or replacements
You may receive up to a 90-day supply of these medications through a participating pharmacy
or mail order service for two Copays (saving you one Copay). It is your responsibility to pay the
Copay amount required each time a prescription is filled.
Mandatory Generic Substitution
All prescriptions will automatically be filled with a Generic Drug where one is available, unless
your Physician indicates the Brand Name Drug must be dispensed (by writing “Dispense as
Written” or “DAW” on your prescription). If your Physician does not indicate “Dispense as Written”
on the prescription for the Brand-Name Drug, and you specifically request the Brand-Name
Drug, you’ll be responsible for paying any difference in cost between the Brand-Name Drug and
the Generic Drug, as well as the Brand-Name Drug Copay.
Mail Order Service
Having your prescriptions filled by mail is easy - Just follow these steps:
For Mail Order: Please dial the RUHS Medical Center Pharmacy main line at 951-486-
4515 and choose Option 5. Mail order turnaround time is usually 3 to 5 business days.
Online Order: Click for Online Order
For the nearest Participating Pharmacy in your area, or additional information regarding the mail
order service, please contact Navitus Customer Care at (866) 333-2757 or the Plan’s Member
Services Department at 800-962-1133 ext. 1.

EPO: 2022
33
Exclusions and Limitations
The Outpatient Prescription Drug Program excludes drugs, medicines and/or related items which
are not covered by the Plan. These items are your financial responsibility. The following are
excluded:
• Drugs or medicines not on the Formulary, unless pre authorized. Pre authorization must
be obtained prior to a prescription being filled --no retro authorizations will be allowed;
• Drugs or medicines purchased and received prior to your effective date or subsequent to
your coverage termination date;
• Therapeutic devices or appliances including hypodermic needles, syringes (except insulin
syringes, other diabetic supplies and syringes for self-injected drugs), support garments
and other non-medicinal substances;
• Non-prescription (over-the-counter) contraceptive jellies, ointments, foams and devices;
• Drugs or medicines to be taken or administered to you while you are a patient in a
Hospital, rest home, nursing home or sanitarium;
• Drugs or medicines delivered or administered to you by a prescriber or the prescriber’s
staff unless approved on a prior authorization as part of the Outpatient Prescription Drug
Program;
• Dietary supplements including vitamins (except prenatal vitamins), fluoride supplements,
health or beauty aids and anorexiants (i.e. diet pills);
• Drugs or medicines for which the cost is recoverable under any workers’ compensation
or occupational disease law, any state or government agency, or furnished by any other
drug or medical service for which no charge is made to you;
• Immunizations, Vaccinations -- for the purpose of travel/vacation;
• Drugs or medicines limited to investigational use or prescribed for experimental or non-
FDA approved indications, unless prescribed in a manner consistent with:
i. A specific indication in “Drug Information Specifications for the Health Care
Professional”, published by the United States Pharmacopoeia Convention;
ii. The American Hospital Formulary Services edition of Drug Information;
iii. Any other source which reflects community practice standards;
• Drugs or medicines available without a prescription (over-the-counter) or for which there
is a non-prescription equivalent available, even if ordered by a Physician;
• Drugs, medicines or cosmetic aids prescribed to primarily improve or otherwise modify
your external appearance;
• Drugs or medicines prescribed by non-Participating Physicians (except for prescriptions
required as a result of an Urgent Care/Urgently Needed Service for an Acute Condition
or prescribed by a licensed dentist);
• Smoking cessation products are limited to one treatment course each Calendar Year
when enrolled in a smoking cessation program;
EPO: 2022
34
• Injectable drugs (except as listed) or;
• Durable Medical Equipment that can be obtained without a prescription.
Dispensing Quantity Limitations
The amount of drug that may be dispensed with each prescription or refill will be in quantities
normally prescribed for up to and including a 30-day supply. Prescriptions requiring greater
amounts will be completed on a refill basis, except as explained under the “Maintenance Drug
Dispensing” section above.
SECTION 7: MENTAL HEALTH/SUBSTANCE ABUSE SERVICES
The Plan provides Benefits for Mental Health, Severe Mental Illness and Substance Abuse
treatment and services.
NOTE: ALL SERVICES MUST BE PRE-AUTHORIZED BY the PLAN’S MEDICAL
MANAGEMENT UNIT.
NO BENEFITS WILL BE PROVIDED FOR TREATMENT OR
SERVICES THAT ARE NOT PRE-AUTHORIZED BY THE PLAN, EXCEPT IN THE CASE OF
PSYCHIATRIC EMERGENCY ADMISSIONS.
Benefits for Mental Health Disorders and Substance Abuse Disorders are outlined in the
“Schedule of Benefits” sections of this SPD. All Services Must Be Pre-Authorized by the
Plan’s Medical Management Unit. Coverage will be provided up to the limits described in the
“Schedule of Benefits”.
Covered Services
The Plan will provide Benefits for the following services furnished in connection with the
treatment of a Mental Health/Substance Abuse Disorder as outlined in the “Schedule of Benefits”
as long as the services are incurred while you are a Member. Services must be pre-authorized
by the Plan’s Medical Management Unit as Clinically Necessary, except in the case of an
emergency Psychiatric Admission.
• Individualized evaluation of needs, referral into treatment and monitoring by a
Participating Mental Health/Substance Abuse Provider;
• Behavioral Health Services provided for Inpatient treatment, treatment at a Residential
Treatment Center or Residential Treatment Facility, and treatment at a Day Treatment
Center;
• Behavioral Health Services provided by a Participating Provider, which are received
at a Participating Facility; Outpatient services provided by a Participating Provider,
except in the case of an emergency Psychiatric Admission;
• Inpatient Detoxification; pre-authorization from the Plan’s Medical Management Unit
is required; limited to hospitalization to remove toxic substances from the system;

EPO: 2022
35
• Nursing by a Registered Nurse, a Licensed Practical Nurse, or a Licensed Vocational
Nurse when Medically Necessary to accompany services provided by a Participating
Provider;
• Participating Practitioner services for individual, group, and family therapy;
• Local ambulance service to and from a facility in the event of an Emergency Condition;
paid based on Allowed Charges;
• Laboratory services authorized by the Plan’s Medical Management Unit or a
Participating Provider, which are related to the approved Behavioral Health Treatment
Plan;
• Psychological testing when pre-authorized by the Plan’s Medical Management Unit
and provided by a licensed, participating psychologist;
• Emergency Treatment;
• Psychotherapy for marital and family problems, when determined Clinically Necessary
by a Participating Mental Health/Substance Abuse Provider; and,
• Treatment for an eating disorder, as defined by the DSM-IV, when pre-authorized by
the Plan’s Medical Management Unit.
What To Do In Emergencies
Whenever possible, you should contact the Plan’s Medical Management Unit before obtaining
Emergency Treatment and services in order to ensure any charges for treatment will be covered.
In some critical emergencies, such as a serious suicide risk, it may not be possible to call the
Plan’s Medical Management Unit before going for treatment. In the event of such an emergency,
you, a family member, or the provider must contact the Plan’s Medical Management Unit
immediately upon admission, or as soon as reasonably possible (within 24 hours).
If you are admitted to any facility without pre-authorization from the Plan’s Medical Management
Unit, upon notification, the Plan’s Medical Management Unit will review the situation by
telephone and conduct a further assessment as appropriate. For Members of the EPO Plan, if
the facility is a non-Participating Facility, you may be transferred to a Participating Facility as
soon as it is medically safe to do so.
Exclusions And Limitations
The following services are excluded:
• Any confinement, treatment, service or supply not pre-authorized by the Plan’s Medical
Management Unit, except for Behavioral Health Services for Emergency Treatment;
• Any confinement, treatment, service or supply provided by a non-Participating Provider,
except for Behavioral Health Services for Emergency Treatment;
• Injury, sickness or disease which arises out of or in the course of any employment, or
which is covered under any workers’ compensation law or similar law;
• Charges incurred while on active duty with the Army, Navy or Air Force of any country or
international organization;
EPO: 2022
36
• Experimental or Investigational Behavioral Health Services and treatment;
• Treatment for any reading or learning disorder, mental retardation, as defined by the
DSM-IV;
• Counseling for adoption, custody, family planning or pregnancy in the absence of a
psychiatric diagnosis generally recognized and accepted by the medical community and
limited to a DSM-IV psychiatric diagnosis;
• Sex therapy, including without limitation, therapy for sexual addiction, in the absence of
a psychiatric diagnosis generally recognized and accepted by the medical community and
limited to a DSM-IV psychiatric diagnosis;
• Pastoral or spiritual counseling;
• Dance, poetry, music or art therapy;
• Non-organic therapies including, but not limited to the following: bio-energetic therapy,
confrontation therapy, crystal healing therapy, educational remediation, Eye Movement
Desensitization and Reprocessing (EMDR), guided imagery, marathon therapy, primal
therapy, Rolfing, sensitivity training, transcendental meditation, Z therapy;
• Organic therapies including, but not limited to the following: aversion therapy, carbon
dioxide therapy, environmental ecological treatment or remedies, herbal therapies,
massage therapy, hemodialysis for schizophrenia, vitamin or orthomolecular therapy,
narcotherapy with LSD, sedative action electrostimulation therapy;
• Private rooms and private duty nursing unless Clinically Necessary as determined by the
Plan’s Medical Management Unit;
• Custodial Care;
• Treatment for caffeine intoxication or dependency on any food substance, in the absence
of a psychiatric diagnosis generally recognized and accepted by the medical community
and limited to a DSM-IV psychiatric diagnosis;
• Services which are required or referred by court order or as a condition of parole or
probation;
• Services which are not Clinically Necessary for the treatment of Mental Health or
Substance Abuse Disorders;
• Treatments designed to regress the Member emotionally or behaviorally;
• Personal enhancement or self-actualization and other non-Clinically Necessary treatment
programs;
• Evaluation or treatment for educational or professional training, investigational purposes
related to employment, fitness for duty evaluations, career/personal counseling;
• Services which are provided by a non-licensed and/or non-qualified practitioner and/or
non-licensed or non-Participating Facility;
• Neurological services and tests, including but not limited to EEG’s, brain scans, MRI’s,
skull x-rays and lumbar punctures for non-diagnosed medical conditions;
• Academic or tutorial programs during treatment at a Residential Treatment Center or
Residential Treatment Facility; or

EPO: 2022
37
• Treatment of organic mental disorders associated with permanent brain dysfunction;
• Behavioral health services that are payable under any state or governmental agency;
• Marriage and Family counseling services performed in connection with conditions not
classified in the DSM-IV;
• Treatment of insomnia and other sleep disorders, dementia, neurological disorders and
other disorders with a known physical basis.
SECTION 8: CHIROPRACTIC CARE BENEFIT
The Plan provides you and your enrolled dependents with a Chiropractic Care Benefit.
Chiropractic services are provided to you through the Plan’s chiropractic provider Network.
How The Chiropractic Care Benefit Works
To begin a course of chiropractic treatment, simply make an initial appointment with the
Participating Chiropractor of your choice. A listing of the Participating Chiropractors can be found
in the provider directory. A referral from your Primary Care Provider is not required for the
initial consultation. At the initial appointment, your chiropractor will collect your Copay. Your
chiropractor will bill the Plan for the remaining charges.
Covered Services
The Chiropractic Care Benefit covers the services described in this section when performed by a
Participating Chiropractor and authorized when necessary by the Plan, up to the annual maximum
benefit listed in the Schedule of Benefits section of this SPD. The following treatment and services
are covered:
• An initial examination and any subsequent examinations, up to a limit of 12 visits per
Calendar Year, with a Participating Chiropractor to determine the nature of your presenting
problem and, if necessary, to prepare a Treatment Plan;
• X-rays and laboratory tests, when prescribed by a Participating Chiropractor,
• X-ray second opinions, only when performed by a Participating Radiologist for verification
of suspected tumors or fractures, and not for routine care;
Exclusions And Limitations
The following items and services are not covered:
• Visits in excess of twelve (12) visits each Calendar Year;
• Service or treatment not authorized by a Participating Chiropractor after the initial
consultation;
• Service or treatment delivered by a non-Participating Chiropractor;
• Services for examination and /or treatment of strictly non neuro-musculoskeletal
disorders;
EPO: 2022
38
• Conjunctive Physical Therapy not associated with spinal or joint adjustment;
• Services not documented as Medically Necessary and appropriate, or classified as
Experimental or Investigational Chiropractic Care;
• Thermography and diagnostic scanning, including Magnetic Resonance Imaging (MRI),
CAT scans, and/or other types of diagnostic scanning;
• Services or treatment for Temporomandibular Joint Disease (TMJ); TMJ is a condition of
the jaw joint which commonly causes headaches, tenderness of the jaw muscles, or dull
aching facial pain;
• Hypnotherapy, behavior training, sleep therapy and weight programs;
• Education programs, non-medical self-care or self-help, or any self-help physical exercise
training, or related diagnostic testing;
• Vitamins, minerals, nutritional supplements or other similar type products;
• Manipulation under anesthesia, hospitalization, anesthesia or any other related services.
SECTION 9: OUT-OF-AREA COVERAGE FOR QUALIFIED DEPENDENTS
How the Out-of-Area Coverage Works
Qualified dependents living outside the EPO Plan Service Area are eligible for the Out-of-Area
Schedule Of Benefits. The qualified dependent may receive treatment and services and seek
reimbursement through the Plan according to the Member Coinsurance and limitations
indicated in the Summary Plan Document. Plan Benefits are paid according to the
reimbursements and limitations shown in the “Out-of-Area Schedule of Benefits” section.
Choice of Providers
As a Member enrolled in this coverage, you may receive treatment and services from any
licensed and qualified provider; then you or your provider may seek reimbursement for Covered
Services by sending the bill to the Plan’s Claims Department. Instructions are included on your
identification card. Be sure to show the provider your identification card when you receive health
care services. The bill will be paid based on the Allowed Charges for the services or treatment
provided. Exclusive Care has contracted with a national re-pricing clearinghouse, to help you
limit your out-of-pocket costs. This re-pricing clearinghouse has contracts with national networks
of participating Hospitals, Physicians and other providers, giving you and Exclusive Care a
discount if your provider participates in one of these networks.
Second Medical Opinion
If you need a second medical opinion, you do not need pre-authorization from Exclusive Care.
However, the second medical opinion must be obtained from an appropriate medical Specialist
and this provider must submit the bill to the Plan with documentation from your initial
consultation. Second medical opinions can only be rendered by a Physician qualified to review
and treat the medical condition in question. If a second medical opinion is deemed not to be
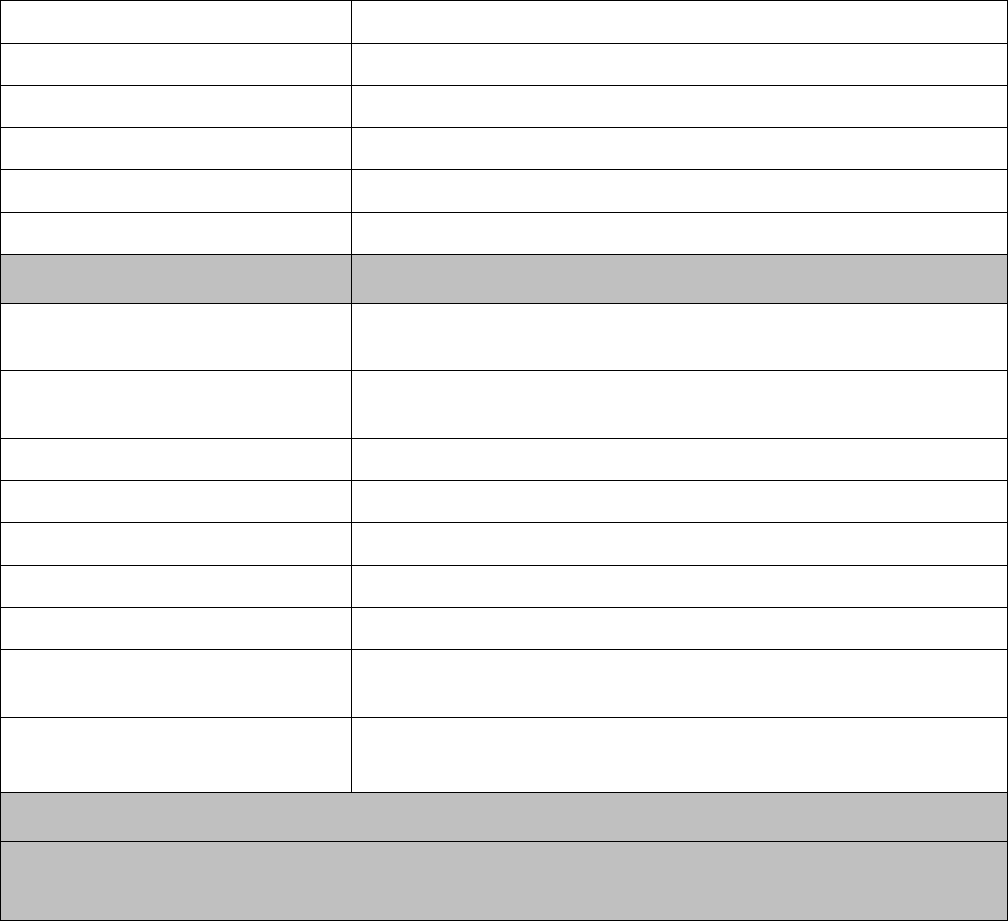
EPO: 2022
39
Medically Necessary and reimbursement is denied, you may appeal the denial by following the
procedures outlined in the “Member Grievance Procedure” section of this SPD. For more
information, please contact the Member Services Department.
The Schedule of Benefits below summarizes the Covered Services that are eligible for
reimbursement and any benefit limitations that apply. Each Member is responsible for payment
of Deductible and Coinsurance amounts as set forth below.
Schedule of Benefits – Out-of-Area Qualified Dependents
Choice of Provider Any licensed and qualified provider
Deductible – Individual $300/Member/Calendar Year
Deductible - Family Not Applicable
Out-of-Pocket-Maximum $5,000/Member/ Calendar Year
Lifetime Maximum Benefit Unlimited
Pre-existing Condition Fully Covered
Outpatient/Office Visits Member Responsibility
Physician Office Visits
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Hospital Clinic Visits
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Periodic Health Evaluations No member responsibility (member pays nothing)
Maternity Care No member responsibility (member pays nothing)
Well Woman Care No member responsibility (member pays nothing)
Well Baby Care No member responsibility (member pays nothing)
Immunizations No member responsibility (member pays nothing)
Diagnostic X-ray & Lab
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Vision Exams (screening and
refractions)
No member responsibility (member pays nothing)
1 Vision Exam per Calendar Year
Outpatient Prescription Drugs
• Prescription Drug Coverage is administered by the Plan’s Pharmacy Benefit Manager (PBM)
• Pharmacy Benefit Manager (PBM): Navitus Health Solutions. Up to 90 Days
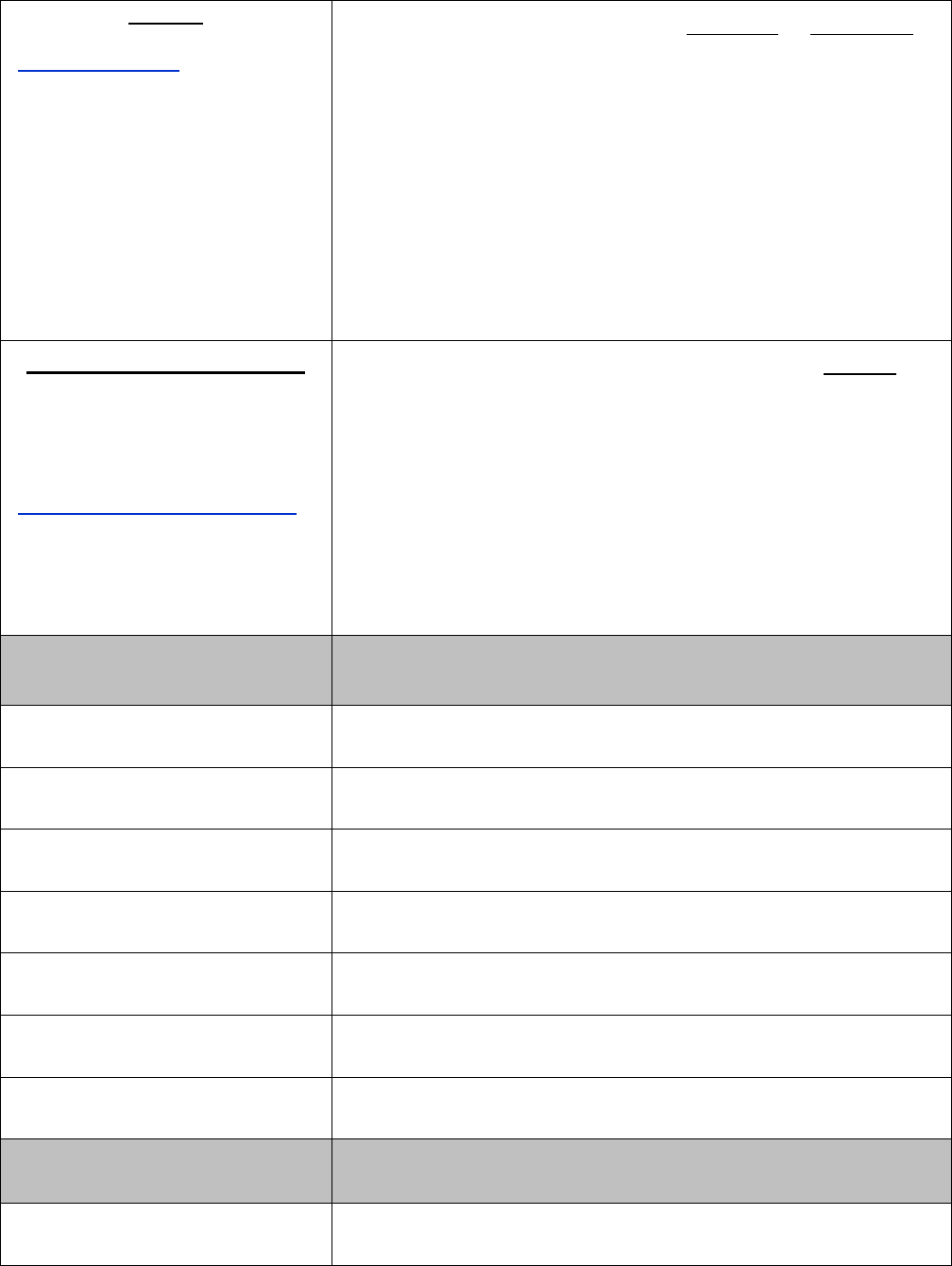
EPO: 2022
40
Navitus
www.navitus.com
Phone: (866) 333-2757
FORMULARY DRUGS
1-34 days
35-90 days
Tier 1; Generic Drugs
$10 Copay
$20 Copay
Tier 2; Preferred Brand Name
Drugs
$25 Copay $50 Copay
Tier 3; Non-
Preferred Brand Name
Drugs
$50 Copay $100 Copay
Significant or new therapeutic class drugs: 50% copay. Some formulary
and all non-formulary drugs require pre-authorization.
Members with Diabetes and Members who use Antihyperlipidemic and
Antihypertensive drugs have no copays for Tier 1 and Tier 2 Supplies
and Medication.
RUHS
- Mail Order Service
Medical Center Retail Pharmacy
26520 Cactus Ave.
Moreno Valley, Ca 92555
Phone (951) 486-4515, option 5
www.ruhealth.org/services/pharmacy
(mail order prescriptions only)
FORMULARY DRUGS
90 days
Tier 1; Generic Drugs
$20 Copay
Tier 2; Preferred Brand Name Drugs
$50 Copay
Tier 3; Non-Preferred Brand Name Drugs
$100 Copay
Significant or new therapeutic class drugs: 50% copay. Some formulary
and all non-formulary drugs require pre-authorization.
Members with Diabetes and Members who use Antihyperlipidemic and
Antihypertensive drugs have no copays for Tier 1 and Tier 2 Supplies
and Medication.
Hospital & Emergency
Room
Member Responsibility
Ambulance (when Medically
Necessary)
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Ambulatory Surgical Center
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Physician Hospital Visits
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Inpatient Hospital Services
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Outpatient Hospital Services
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Hospital Emergency Services
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Urgent Care/Urgently Needed
Services
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Severe & Non-Severe
Mental Health Treatment
Member Responsibility
Inpatient Care
20% of Allowed Charges (and any amount in excess of
Allowed Charges)

EPO: 2022
41
Outpatient Care - Individual
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Outpatient Care - Group
Substance Abuse
Treatment
Member Responsibility
Inpatient Care
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Inpatient Detoxification
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Outpatient Hospital Services
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Outpatient Office Visit
Other Benefits Member Responsibility
Allergy Testing & Treatment
20% of Allowed Charges (and any amount in excess of
Allowed Charges)
Chiropractic Care
20% of Allowed Charges (and any amount in excess
of Allowed Charges); Benefits limited to 12
visits/Calendar Year
Members Requiring Diabetes
Care
Pharmacy Copays are waived for all Generic and
Preferred Brand Name Formulary injectable and oral
antidiabetic medications and diabetic supplies
(testing strips, syringes, etc.)
Members Taking
Antihyperlipidemic and
Antihypertensive Drugs
Pharmacy Copays are waived for all Generic and
Preferred Brand Name antihyperlipidemic and
antihypertensive Drugs
Durable Medical Equipment
50% of Allowed Charges (and any amount in excess
of Allowed Charges);
Other Medical Equipment 20% of Allowed Charges
Family Planning
Elective Pregnancy
Termination
Infertility Services
Tubal Ligation
Vasectomy
20% of Allowed Charges (and any amount in excess
of Allowed Charges) ; (3
rd
trimester only covered if
pregnancy life-threatening to mother)
50% of Allowed Charges (and any amount in excess
of Allowed Charges); up to a maximum of $10,000
lifetime benefit
20% of Allowed Charges (and any amount in excess
of Allowed Charges)
20% of Allowed Charges (and any amount in excess
of Allowed Charges)
Home Health Care
20% of Allowed Charges (and any amount in excess
of Allowed Charges)

EPO: 2022
42
Hospice Care
20% of Allowed Charges(and any amount in excess
of Allowed Charges)
Physical Therapy
20% of Allowed Charges (and any amount in excess
of Allowed Charges); up to 30 visits/Disability within a
90day period
Skilled Nursing Facility
20% of Allowed Charges (and any amount in excess
of Allowed Charges); up to 100 days/Disability
Hearing Aid Instrument $3,000/Member; once every 36 months
An explanation of terms used in this Schedule of Benefits follows below, to help you get
the most from your Out-Of-Area coverage:
Pre-Existing Conditions
The Plan has no pre-existing conditions limitation. Therefore, there are no limitations, waiting
periods or exclusions for being treated for any diagnosis or condition currently on record for you
as long as services are Covered Services.
Medically Necessary
The Plan only covers Medically Necessary health care services. See the Section “Definition of
Terms” in this SPD for a more detailed explanation. Certain services require a medical review
by the Plan’s Medical Management Unit, to establish whether or not the services were Medically
Necessary.
Allowed Charges
For services provided by a non-Participating Provider, the Plan’s reimbursement to the provider
is based on an Allowed Charge, which is consistent with the current rate or charge for the service
being rendered, in a certain geographic area, for identical or similar services, as determined by
the Plan and subject to all other terms of this Summary Plan Document.
Copay
The amount you are required to pay for certain Covered Services identified in the Schedule of
Benefits above. You may be required to pay the Copay amount to the provider before the
provider submits a bill to the Plan. In the case of outpatient prescription drugs, you are always
required to pay the Copay amount at the time a prescription is filled. The Plan pays for Covered
Expenses up to the Allowed Charge, subject to all other terms and limitations described in the
Schedule of Benefits, General Provisions, or Exclusions and Limitations sections of this SPD.
Deductible – Individual/Family
The Deductible is the portion of the cost of medical expenses you must pay each Calendar Year
before the Plan will pay any Benefits.
Out-of-Pocket Maximum
The Plan helps protect you from costly medical expenses by limiting the total amount you pay
out of your own pocket for certain services in any one Calendar Year. When the amount that
EPO: 2022
43
you or any enrolled dependent has paid for these services reaches the designated level (the
Out-of-Pocket Maximum), you will pay nothing further for Covered Services for the rest of the
Calendar Year (up to any benefit maximums that may apply). Out-of-Pocket amounts you pay
which do not count towards each Member’s Out-of-Pocket Maximum include:
• Deductibles
• Charges in excess of the Allowed Charges covered by the Plan;
• Charges for services that are not covered by the Plan, such as a charge for a service
listed as an exclusion;
• Charges for services for which no benefit is payable because the dollar or benefit limit
has been exceeded;
Lifetime Maximum Benefit
Unlimited
Member Liability
In the event the Plan fails to pay a provider for Covered Services, you will not be liable to the
provider for any sums owed by the Plan based on the Summary Plan Document. You will be
financially liable for any amounts owed to a provider who does not accept payment based on
the Allowed Charges reimbursed by the Plan for services rendered. In addition, all Member
Deductibles, the percentage amounts listed (e.g. 20% of Allowed Charges), and dollar Copay
amounts (e.g. $15 Copay), are always your responsibility.
If you have any questions about your Out-of-Area coverage, contact the Member Services
Department: (800) 962-1133, option 1, 8:00 a.m. - 5:00 p.m. Monday through Friday, Pacific
Coast Time.
This Summary Plan Document will be the primary governing document for all Plan coverage
decisions and will be the basis for final determination of reimbursements. This Health Plan is
intended to comply with all laws and regulations that are applicable whether or not specifically
described in this Summary Plan Document.
SECTION 10: PLAN GENERAL PROVISIONS
Claim Payment Procedures
The Plan is designed to eliminate claim forms and limit your out-of-pocket expenses other than
required Deductibles. In some circumstances, you may incur expenses for Covered Services
(such as for out-of-area Emergency Care services). If this happens, submit a copy of the bill and
your receipt to the Claims Department, and the Plan will reimburse you for those expenses
according to the Plan’s Benefits, minus any applicable Copay amounts that are your
responsibility.
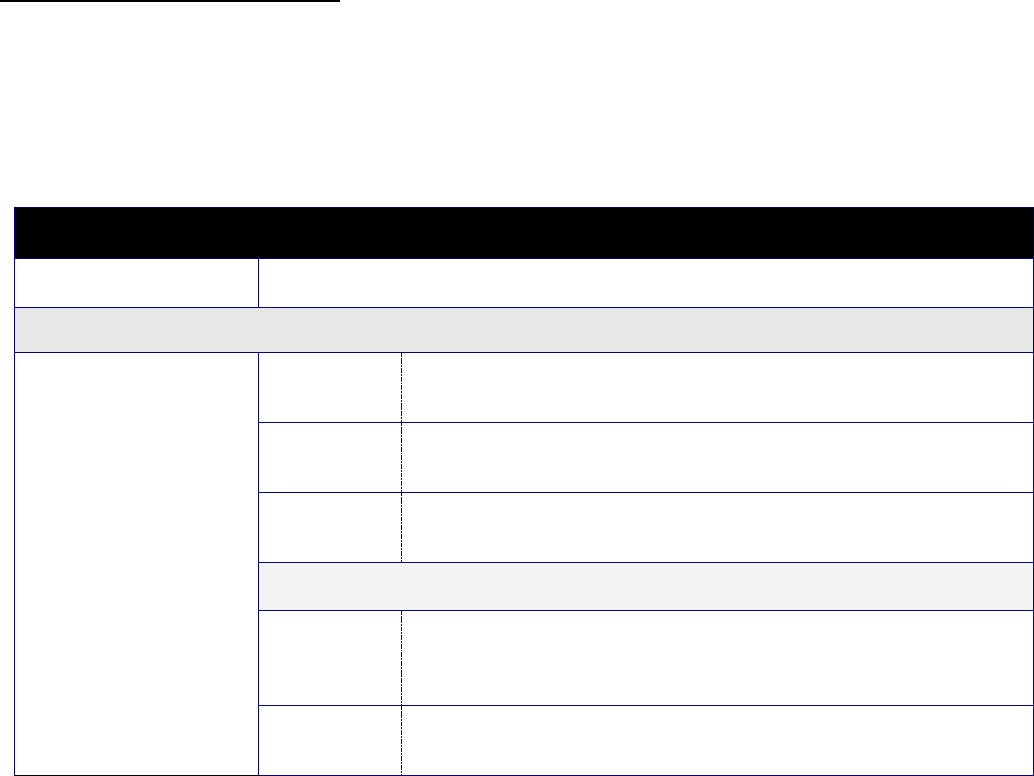
EPO: 2022
44
If you receive a bill for Covered Services that you believe should have been paid by the Plan, a
copy of the bill must be submitted within 90 days of the date the service was rendered to:
EXCLUSIVE CARE Claims Department
P.O. Box 1508
Riverside CA 92502
Failure to submit bills within the time required shall not invalidate nor reduce any claim if it was
not reasonably possible to submit the bill within that time, provided proof of the billing is
furnished as soon as reasonably possible. However a bill will not be accepted, except in the
absence of legal capacity, later than one year from the time proof of the billing is otherwise
required.
In the event such a claim is denied, you may resubmit within 180 days of the initial denial,
explaining in writing why you believe your claim should be approved. Your request will be
considered a formal grievance and handled under the “Member Grievance Procedure” section
described below.
Member Grievance Procedure
If a pre-authorization request or a claim for Benefits is denied in whole or in part, you may
appeal the decision by contacting Exclusive Care at the above address. The following chart
outlines the responsibilities of the Plan and of the Member, during the appeal process, and the
steps taken to ensure the appeal is administered according to the Plan’s Member Grievance
Procedure:
Service Authorization, Claims Review and Appeal Chart
Type of Transaction
Steps to Take
PRE AUTHORIZATION FOR URGENT HEALTH CARE SERVICES
Pre authorizations for
conditions that could
jeopardize life, health, or
ability to regain maximum
function, or would subject
you to severe pain.
The reasonable layperson
standard is used for these
claims, except that if a
Physician determines the
condition is urgent, the
Plan must accept the
Physician’s determination.
Step 1:
The Plan has 72 hours after receiving your initial pre authorization request
to notify you if your request is approved or denied.
Step 2: If denied, you have 180 days after receiving the pre authorization denial to
appeal the Plan’s decision.
Step 3: The Plan has 72 hours after receiving your appeal to notify you of its
decision.
I
F
Y
OUR PRE AUTHORIZATION REQUEST IS
I
MPROPERLY
F
ILED OR
I
NCOMPLETE
Step 1:
The Plan has 24 hours after receiving your initial pre authorization request
to notify you that your pre authorization request is improperly filed or
incomplete.
Step 2:
You have
48 hours
after receiving notice from the Plan to correct or
complete your pre authorization request.
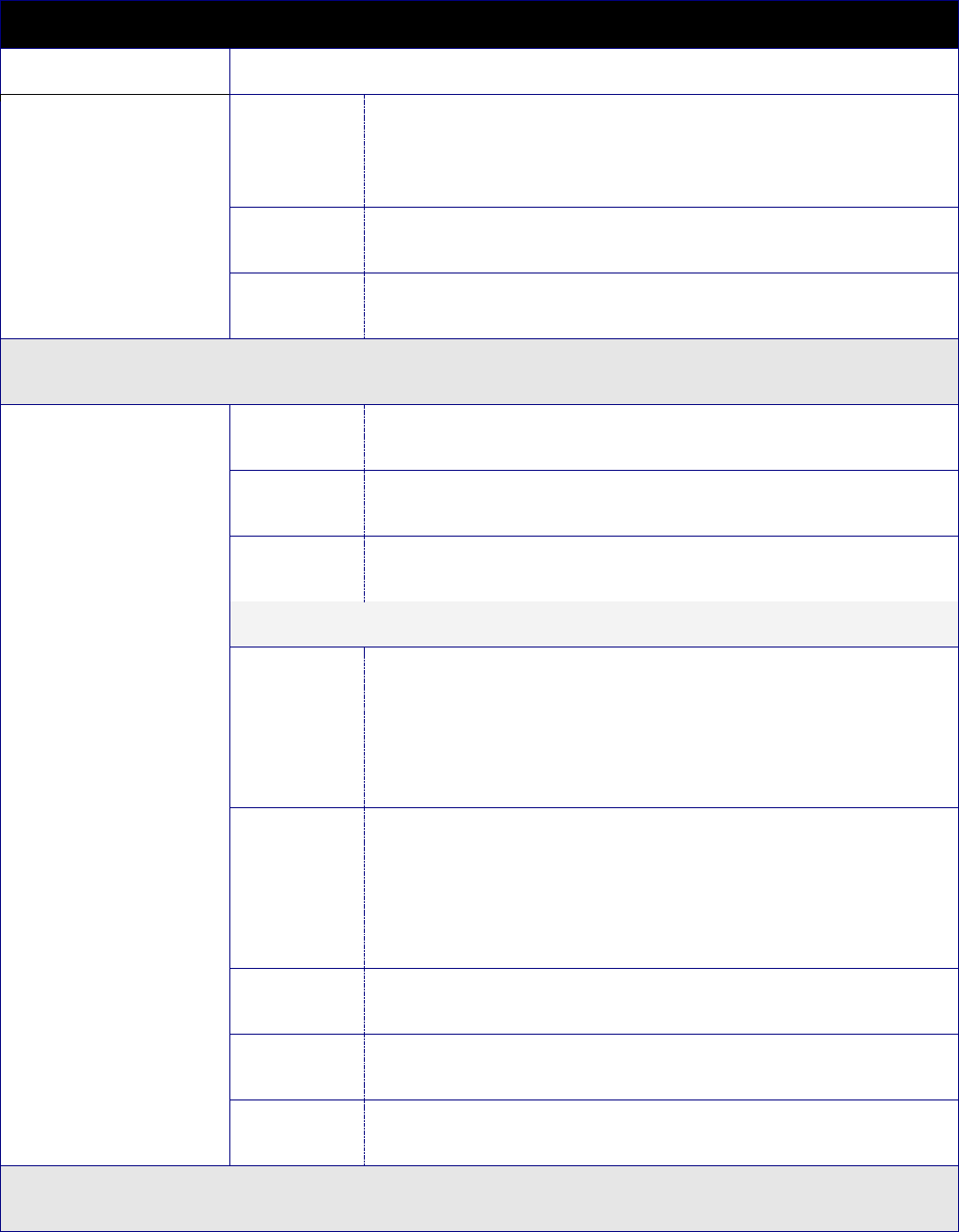
EPO: 2022
45
Service Authorization, Claims Review and Appeal Chart
Type of Transaction
Steps to Take
Step 3:
The Plan has 48 hours to notify you if your pre authorization request is
approved or denied. The Plan must do so within the earlier of 48 hours of:
Receiving your corrected/completed pre authorization request, or your
deadline to complete the pre authorization request.
Step 4:
If denied, you have 180 days after receiving the pre authorization denial to
appeal the Plan’s decision.
Step 5:
The Plan has 72 hours after receiving your appeal to notify you of its
decision.
PRE AUTHORIZATION FOR HEALTH CARE SERVICES
Pre authorization requests
for Benefits under this Plan
where treatment must be
authorized before it is
performed.
Step 1:
The Plan has 15 days after receiving your initial pre authorization request to
notify you if your request is approved or denied.
Step 2:
You have 180 days after receiving the pre authorization denial to appeal the
Plan’s decision.
Step 3:
The Plan has 30 days after receiving your appeal to notify you of its
decision.
IF YOUR PRE AUTHORIZATION REQUEST IS IMPROPERLY FILED OR INCOMPLETE
Step 1:
As long as your pre authorization request is received by a person or
organizational unit customarily responsible for handling pre authorizations,
and it names a specific Member, a specific medical condition or symptom,
and a specific treatment, service, or product for which approval is
requested, the Plan has 5 days after receiving your initial pre authorization
request to notify you that your request is improper or incomplete.
Step 2:
The Plan has 15 days after receiving your pre authorization request to notify
you of its decision to approve or deny the pre authorization request. If the
Plan needs more information and provides an extension notice during the
initial 15-day period, it has 30 days after receiving the pre authorization
request to notify you of its decision. (The time the Plan waits for requested
additional information is not counted in totals.)
Step 3:
You have 45 days after receiving the extension notice to provide additional
information or complete the pre authorization request.
Step 4:
If your pre authorization is denied, you have 180 days after receiving the
pre authorization denial to appeal the Plan’s decision.
Step 5:
The Plan has 30 days after receiving your appeal to notify you of its
decision.
POST-SERVICE HEALTH CARE CLAIMS
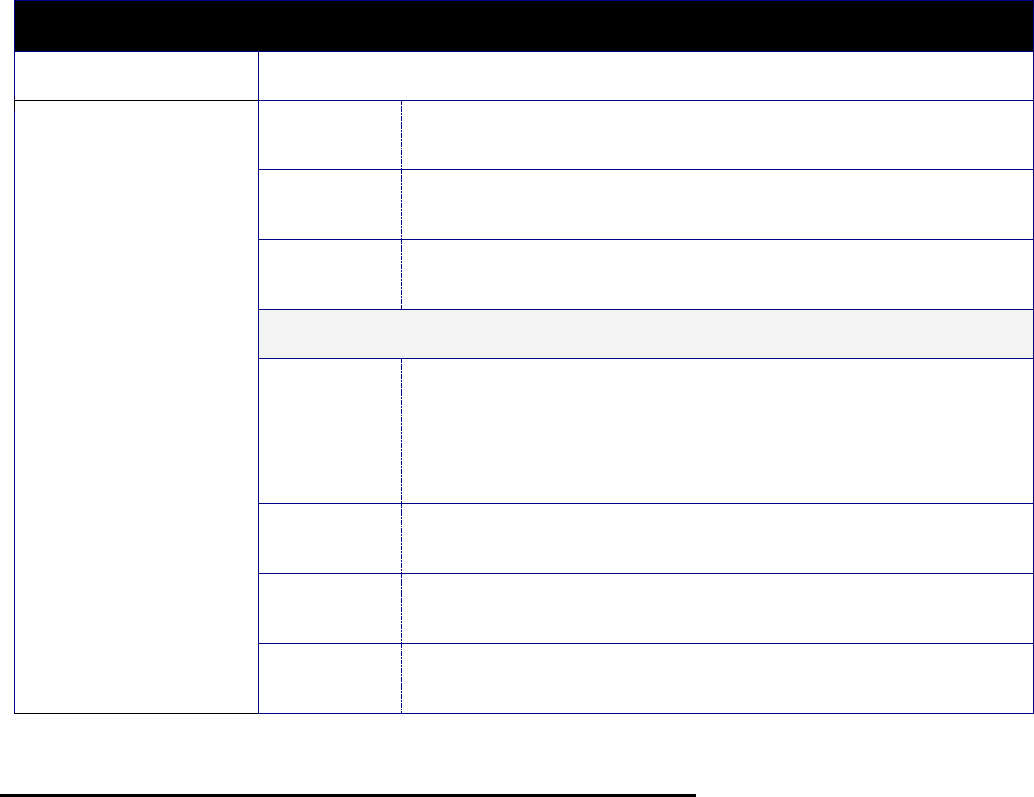
EPO: 2022
46
Service Authorization, Claims Review and Appeal Chart
Type of Transaction
Steps to Take
Claims for Benefits where
healthcare services have
already been received by
the Member.
Step 1:
The Plan has 30 days after receiving your initial claim to notify you if your
claim is denied.
Step 2:
If your claim is denied, you have 180 days after receiving the claim denial to
appeal the Plan’s decision.
Step 3:
The Plan has 60 days after receiving your appeal to notify you of its
decision.
I
F THE
P
LAN
N
EEDS
F
URTHER
I
NFORMATION OR AN
E
XTENSION
Step 1:
The Plan has 30 days after receiving the initial claim to notify you if your
claim is denied. If the Plan needs more information and provides an
extension notice during the initial 30-day period, it has 45 days after
receiving the claim to notify you if your claim is denied. (The time the Plan
waits for requested additional information is not counted in totals.)
Step 2:
You have 45 days after receiving the extension notice to provide the
requested additional information or complete your claim.
Step 3:
If your claim is denied, you have 180 days after receiving the claim denial to
appeal the Plan’s decision.
Step 4:
The Plan has 60 days after receiving your appeal to notify you of its
decision.
Pre Authorization Denials / Claim Denials - Appeal Procedure
If your pre authorization request or claim for Benefits is wholly or partially denied, any pre
authorization denial / claim denial notice you receive will:
• State the specific reasons for the decision;
• Reference specific Plan provisions on which the decision is based;
• Describe additional material or information necessary to complete the pre-
authorization request or claim request, and why such information is necessary; and
• Describe Plan procedures and time limits for appealing the decision, and your right to
obtain information about those procedures.
The pre authorization denial / claim denial notice will also:
• Disclose any internal rule, guidelines, protocol or similar criterion relied on in making
the decision (or state that such information will be provided free of charge upon
request);
• Provide an explanation of the scientific or clinical judgment for the decision, applying
layperson terms to your medical condition, if the denial is based on Medical Necessity

EPO: 2022
47
or Experimental or Investigational treatment (or state that such information will be
provided free of charge upon request); and
• Include a description of the expedited review process applicable to Urgent Care pre-
authorizations. This denial may be given orally, provided that a written or electronic
notification is furnished to you no later than 3 days after the oral notification.
If you believe your pre authorization request or claim was denied in error, you may appeal this
decision. You have 180 days after receiving the denial to appeal the Plan’s decision. You may
submit written comments, documents, or other information to the Plan in support of your appeal
and have access, upon request, to all relevant documents free of charge. The review by the
Plan of the initial denial will take into account all new information, whether or not presented or
available at the initial pre authorization/claim review, and will not be influenced by the initial
decision.
A person other than the person who made the initial pre authorization or claim denial will conduct
the appeal review and will not work under the original decision maker’s authority. If your claim
was denied on the grounds of Medical Necessity, the Plan will consult with a Health Care
Professional with appropriate training and experience. This Health Care Professional will not be
the individual who was consulted during the initial decision and will not work under his/her
authority.
If your pre authorization request or claim involves Urgent Care, a request for an expedited appeal
may be submitted orally or in writing and all necessary information shall be transmitted between
the Plan and you by telephone, fax, or other similar method.
Outcome of Appeal Procedure
If your appeal is denied, the appeal denial notice will contain the following information:
• The specific reasons for the appeal denial;
• A reference to the specific Plan provisions on which the denial was based;
• A statement that you are entitled to receive upon request, and without charge,
reasonable access to or copies of all document, records, or other information relevant
to the appeal denial;
• A statement describing any additional voluntary appeal procedures offered by the Plan
and your right to obtain information about these procedures.
The appeal denial notice will also include:
• A statement disclosing any internal rule, guidelines, protocol or similar criterion relied
on in making the decision (or a statement that such information will be provided free
of charge upon request);
• An explanation of the scientific or clinical judgment for the decision, if the denial is
based on Medical Necessity or Experimental or Investigational treatment, applying
layperson terms to your medical condition (or state that such information will be
provided free of charge upon request);
• A statement that “You or your plan may have other alternative dispute resolution
options”, such as Neutral Binding Arbitration. The appeal denial notice may be
EPO: 2022
48
provided in written or electronic form. Electronic notices will be provided in a form that
complies with any applicable legal requirements.
Member Services Responsibilities
Member services representatives answer all incoming Member calls and explain the Plan
Benefits and applicable policies and procedures. Upon receiving a Member’s complaint, a
member services representative will gather as many facts as possible and attempt to reach a
resolution with the Member. If the complaint is something that cannot be resolved through the
clarification of Benefits or further education about the Plan, the member services representative
will inform the Member of his/her right to submit a Member grievance form for further
consideration. The grievance form must contain the facts surrounding the circumstances and
must be submitted by the Member to the Member Services Department listed on the form.
Administrative Review Committee Responsibilities
The Administrative Review Committee will respond to all written grievances related to
operational and non-clinical issues within 30 days of receipt of the written grievance.
Physician Review Committee Responsibilities
The Physician Review Committee will respond to all written grievances related to clinical issues
within the specified timeframes outlined in the “Service Authorization, Claims Review and Appeal
Chart” in this section.
Experimental or Investigational Treatment Of Terminal Illness
If the Plan’s Medical Director denies a treatment as Experimental or Investigational (refer to the
Plan’s “Specific Exclusions” section) for a Member who has a terminal illness, the Plan, at the
Member’s request, will hold a Physician Review Committee within thirty (30) days of the receipt of
the request to review the denial and the basis for determining that the proposed treatment or
services are Experimental or Investigational. The review will be held within five (5) days if the treating
Physician determines, in consultation with the Medical Director, based on standard medical practice,
that the effectiveness of either the proposed treatment or services would be materially reduced if not
provided at the earliest possible date.
If the denial is appealed, the Medical Director or other appropriately licensed health care provider
will only review the appeal if he/she determines that he/she is competent to evaluate the specific
clinical issues presented in the appeal. If the Medical Director or health care provider determines
that he/she is not competent to evaluate the specific clinical issues of the appeal, a
review/consultation will be obtained from an appropriately licensed health care provider or
Specialist who has the education, training, and relevant expertise that is pertinent to evaluating
the clinical issues underlying the appeal. Appeals include claims that are denied: (1) on the basis
of a clinical issue; (2) on the basis of the necessity for treatment, or (3) on the basis of the type
of treatment proposed or utilized.
Alternative Dispute Resolution

EPO: 2022
49
If no resolution to your complaint is achieved by the Plan’s internal Member Grievance
Procedure, you have several options depending on the nature of your complaint:
Eligibility Issues
This matter must be referred directly to your employer group.
Malpractice
You must proceed directly to court regarding issues of malpractice.
Bad Faith
You must proceed directly to court regarding issues of bad faith.
Independent Medical Review of Grievances Involving Disputed Health Care Services
You may request an independent medical review ("IMR") of disputed health care services if you
believe that health care services eligible for coverage and payment under your Exclusive Care
Plan have been improperly denied, modified or delayed by Exclusive Care or one of its
contracting providers. A "Disputed Health Care Service" is any health care service eligible for
coverage and payment under your Exclusive Care Plan that has been denied, modified or
delayed by Exclusive Care or one of its contracting providers, in whole or in part because the
service is not Medically Necessary.
The IMR process is in addition to any other procedures or remedies that may be available to
you. You pay no application or processing fees of any kind for IMR. You have the right to provide
information in support of the request for IMR. Exclusive Care will provide you with an IMR
application form and Exclusive Care’s grievance response letter that states its position on the
Disputed Health Care Service. A decision not to participate in the IMR process may cause you
to forfeit any statutory right to pursue legal action against Exclusive Care regarding the Disputed
Health Care Service.
Eligibility for Independent Medical Review
Your application for IMR will be reviewed by the IMR organization to confirm that it meets all the
eligibility requirements of the law for IMR which are set out below:
1. Your provider has recommended a health care service as Medically Necessary; or you
have received urgent or Emergency Care that a provider determined to have been
Medically Necessary. In the absence of the provider recommendation described above,
you have been seen by an Exclusive Care Member Physician for the diagnosis or
treatment of the medical condition for which you seek IMR;
2. The Disputed Health Care Service has been denied, modified or delayed by Exclusive
Care or one of its contracting providers, based in whole or in part on a decision that the
health care service is not Medically Necessary; and
3. You have filed a grievance with Exclusive Care and the disputed decision is upheld by
Exclusive Care or the grievance remains unresolved after 30 days. Within the next six
months, you may apply for IMR or later, if the IMR agrees to extend the application

EPO: 2022
50
deadline. If your grievance requires expedited review you may bring it immediately to the
attention of the IMR. The IMR may waive the requirement that you follow Exclusive Care’s
grievance process in extraordinary and compelling cases. If your case is eligible for IMR,
the dispute will be submitted to a medical specialist who will make an independent
determination of whether or not the care is Medically Necessary.
You will receive a copy of the assessment made in your case from the IMR. If the IMR determines
the service is Medically Necessary, Exclusive Care will provide benefits for the Disputed Health
Care Service. If your case is not eligible for IMR, the IMR will advise you of your alternatives.
For non-urgent cases, the IMR organization must provide its determination within 30 days of
receipt of the application for review and the supporting documents. For urgent cases involving
imminent and serious threat to your health, including, but not limited to, serious pain, the potential
loss of life, limb or major bodily function or the immediate and serious deterioration of your health,
the IMR organization must provide its determination within three business days. For more
information regarding the IMR processor to request an application form, please call Exclusive
Care’s Member Services Department at the telephone number on your Exclusive Care ID Card.
Neutral Binding Arbitration
Arbitration is an alternative method of resolving disputes in which two parties present their
individual sides of a complaint to an objective arbitrator or panel of arbitrators, who will weigh
the facts and arguments of both parties and resolve the dispute.
Exclusive Care uses neutral binding arbitration to resolve disputes. By enrolling
in the Plan, you are waiving your rights to a jury or court trial for disputes. These
disputes will be settled by neutral binding arbitration.
State of California Laws regarding Arbitration
Arbitration is a vehicle for the resolution of any disputes concerning health care services,
Benefits, or contract interpretation pertaining to any personal liability, tort claims, or contract
disputes originating from Exclusive Care’s employer group agreement. Personal liability, tort
claims, or contract disputes related to eligibility for enrollment, effective date of coverage, and
malpractice or bad faith are EXCLUDED from binding arbitration. For allegations of bad faith or
malpractice, proceed directly to the appropriate court. Arbitration will be held in the County of
Riverside.
Costs associated with the services of the named Arbitrator will be shared by the parties involved.
Costs for individual preparation and/or attendance (complaining parties, witnesses, travel
expenses. etc.) at the arbitration will be the sole responsibility of the party incurring the expense.
Pursuant to California law, any claim of up to $200,000 must be decided by a single neutral
arbitrator who shall be chosen by the parties and who shall have no jurisdiction to award more
than $200,000.
However, Exclusive Care and the Member may agree in writing to waive the requirement to use
a single arbitrator and instead opt to use a tripartite arbitration panel that includes the two-party
appointed arbitrators or a panel of three neutral arbitrators, or another multiple arbitrator system
mutually agreeable to the parties. You have three (3) business days to rescind the waiver
EPO: 2022
51
agreement unless the agreement has also been signed by your attorney, in which case the
waiver cannot be rescinded.
In cases of extreme hardship, Exclusive Care may assume all or part of your share of the fees
and expenses of the neutral arbitrator provided you submitted a hardship application to the
American Arbitration Association. The approval or denial of a hardship application shall be
determined by the American Arbitration Association. You may obtain a hardship application by
contacting the American Arbitration Association at (800) 778-7879.
If you have a grievance against Exclusive Care, you should first telephone Exclusive Care at 1-
800-962-1133 and use Exclusive Care's grievance process. Utilizing this grievance process
does not prohibit any potential legal rights or remedies that may be available to you. You may
also be eligible for an Independent Medical Review (IMR). If you are eligible for IMR, the IMR
process will provide an impartial review of medical decisions made by Exclusive Care related to
the Medical Necessity of a proposed service or treatment, coverage decisions for treatments
that are Experimental or Investigational in nature and payment disputes for emergency or urgent
medical services.
COBRA Continuation of Coverage
Under the terms of the Consolidated Omnibus Budget Reconciliation Act (COBRA), continued
coverage is available to a qualified beneficiary should he/she lose coverage under the
circumstances described below. Each COBRA-eligible person has a right to make a separate
election—choosing or declining COBRA coverage—when there is a qualifying event that causes
loss of coverage under the Plan.
Qualified Beneficiaries
A qualified beneficiary generally is an individual covered by a group health plan on the day before
a qualifying event occurs who is an employee, the employee's spouse, or an employee's
dependent child. In certain cases, a retired employee, the retired employee's spouse, and the
retired employee's dependent children may be qualified beneficiaries. In addition, any child born
to or placed for adoption with a covered employee during the period of COBRA coverage is
considered a qualified beneficiary. Agents, independent contractors, and directors who
participate in the group health plan may also be qualified beneficiaries.
Qualifying Events
Qualifying events are certain events that would cause an individual to lose health coverage.
The type of qualifying event will determine who the qualified beneficiaries are and the amount
of time that a plan must offer the health coverage to them under COBRA. A plan, at its
discretion, may provide longer periods of continuation coverage.
Qualifying Events for Employees:
Voluntary or involuntary termination of employment for reasons other than gross
misconduct;
Reduction in the number of hours of employment.
Qualifying Events for Spouses:
EPO: 2022
52
Voluntary or involuntary termination of the covered employee's employment for any
reason other than gross misconduct;
Reduction in the hours worked by the covered employee;
Covered employee becoming entitled to Medicare;
Divorce or legal separation of the covered employee;
Death of the covered employee.
Qualifying Events for Dependent Children:
Loss of dependent child status under the Plan rules;
Voluntary or involuntary termination of the covered employee's employment for any
reason other than gross misconduct;
Reduction in the hours worked by the covered employee;
Covered employee becoming entitled to Medicare;
Divorce or legal separation of the covered employee;
Death of the covered employee.
If a qualified beneficiary chooses COBRA continuation coverage, his/her Benefits will be the
same as the coverage he/she had under the Plan prior to coverage termination. The qualified
beneficiary pays the full premium cost of continuation coverage, plus any additional amounts
permitted by law. If benefit levels and/or rates change for Plan Members, the qualified beneficiary
will be subject to those same changes. COBRA coverage for each of the above qualifying events
will continue for up to 36 months from the date of the qualifying event unless COBRA is canceled
for any one of the reasons specified below under “Canceling COBRA Coverage.”
COBRA Notice Requirement
A qualified beneficiary must notify his/her employer group or its designee prior to the qualifying
event, or as soon as possible thereafter and not more than 30 days after the qualifying event.
When the employer group or it designee receives notice, it must in turn notify you, any spouse
and/or children (individually or jointly) of your and their right to elect COBRA coverage by
sending COBRA continuation information and a COBRA election form, within thirty (30) days of
the qualifying event.
You may enroll newly acquired, adopted or newborn children into your COBRA coverage if you
notify the employer group or its designee within 30 days of the birth or placement for adoption.
COBRA Election Deadline
To elect COBRA coverage, you must submit a completed COBRA election form to your employer
group or its designee within 60 days after receiving the election form or, if later, 60 days after
coverage under the Plan would otherwise end if COBRA coverage was not elected. Your spouse
or children cannot elect COBRA coverage after the expiration of this 60-day deadline.
The Benefits under COBRA are identical to the Plan Benefits offered at the time of the qualifying
event and the Cost Of Coverage, under the initial COBRA term, may not exceed 102% of the
current group premium.
EPO: 2022
53
COBRA coverage may be extended for up to an additional eleven (11) months if the covered
individual is recognized by the Social Security Administration as disabled, but not yet Medicare
eligible. This extension of COBRA coverage is available at a cost not to exceed 150% of the
current group premium and may become effective after the initial 36 months of coverage is
exhausted.
Canceling COBRA Coverage
If you choose COBRA, your coverage will be canceled in less than 36 months if:
Payments for the COBRA coverage are not paid on a timely basis. To be timely, a
payment must be paid within 30 days of its due date (or 45 days of the due date for the
initial payment);
You become covered under another group health plan. However you may continue
COBRA coverage if the other group health plan limits coverage for pre-existing medical
conditions that your spouse or children may have;
You become enrolled in Medicare;
The Plan terminates;
COBRA Coverage - Bankruptcy Provision
Under COBRA, continued coverage is available in the event that a County bankruptcy
proceeding causes a loss of coverage (including a substantial elimination of coverage within one
year before or after the bankruptcy proceeding commences). As a Plan Member, you are eligible
for this continuation coverage if you enrolled in the Plan before the substantial elimination of
coverage occurred. As a dependent participating in the Plan, you are eligible for this continuation
coverage if, on the day before the bankruptcy, you were covered under the Plan as a spouse,
dependent child, or surviving spouse.
COBRA coverage also continues under these circumstances, as follows:
Affected retirees and surviving spouses of deceased retirees may elect lifetime COBRA
coverage;
Spouses and dependent children may continue COBRA coverage until the retiree dies;
When the retiree dies, his/her surviving spouse and dependent children may elect an
additional 36 months of COBRA coverage commencing with the date of the retiree’s
death. Coverage could end sooner if COBRA coverage otherwise ends (e.g., due to
nonpayment of premiums or discontinuation of all group health coverage by the County);
however, the maximum COBRA coverage period will not expire due to Medicare
entitlement.
If you have any questions about these laws, please contact the County of Riverside Benefits
Division or your employer group or its designee.

EPO: 2022
54
Health Insurance Portability and Accountability Act (HIPAA)
The following is Exclusive Care’s “Notice of Privacy Practices” statement governing Exclusive
Care’s use of Members’ health information which Exclusive Care is required by federal law to
provide to its Members:
Exclusive Care – Notice of Privacy Practices
Exclusive Care creates records of health care to provide quality care and comply with legal
requirements. Exclusive Care understands your health information is personal and private, and
commits to safeguarding it to the extent reasonably possible. This individually identifiable health
information is known as “protected health information” (PHI). Exclusive Care is required by law
to:
• Assure that health information that identifies you is kept private;
• Give you notice of Exclusive Care’s legal duties and privacy practices with respect to your
health information;
• Notify you if you are affected by a breach of unsecured PHI; and
• Follow the terms of this notice currently in effect.
This notice outlines the limits on how Exclusive Care will handle your health information.
Under federal law, Exclusive Care must provide a copy of this notice when you receive health
care and related services from Exclusive Care, or participate in certain health plans
administered or operated by Exclusive Care. Exclusive Care reserves the right to change
practices and make new provisions effective for all health information it maintains. Exclusive
Care retains all final authority and responsibility for the Plan and its operations, including Plan
privacy policies, practices and procedures. Exclusive Care will interpret and construe the
benefits of the Plan in accordance with current laws and regulations as identified in this notice
and as amended from time to time. You may request an updated copy of this notice at any
time.
A. Use and Disclosure – General
Generally, except as otherwise specified below, Exclusive Care may use and disclose the
following health information, as allowed by state and federal law:
1. For treatment. Exclusive Care uses and discloses health information to provide you with
health care and related services. For instance:
• Nurses, doctors, or other Exclusive Care employees may record your health
information, and they may share such information with other Exclusive Care
employees.
• Exclusive Care may disclose health information to people outside Exclusive Care
involved in your care who provide treatment and related services.
• Exclusive Care may use and disclose health information to contact you to remind
you about appointments for treatment or health care-related services.
• In emergencies, Exclusive Care may use or disclose health information to provide
you treatment. Exclusive Care will make its best effort to obtain your permission
to use or disclose your health information as soon as reasonably practical.
EPO: 2022
55
2. For payment. Exclusive Care may bill you, insurance companies, or third parties.
Information on or accompanying these bills may identify you, as well as diagnoses,
assessments, procedures performed, and medical supplies used.
3. For health care operations. Exclusive Care may use information in your health record
to assess the care and outcomes in your case to improve our services, and in
administrative processes such as purchasing medical devices, or for auditing financial
data. Exclusive Care may combine health information about many plan members in
summary format with the purpose of analyzing plan coverage for plan sponsors.
4. For health plan administration. As administrator of certain health plans, such as
Medicare, Medi-Cal, and Exclusive Care, Exclusive Care may disclose limited health
information to plan sponsors. The law only allows using such information for purposes
such as plan eligibility and enrollment, benefits administration, and payment of health
care expenses. The law specifically prohibits use for employment-related actions or
decisions.
B. Use and Disclosure Requiring Your Authorization
On a limited basis, Exclusive Care may use and disclose health information only with your
permission, as required by state and federal law:
1. From mental health records.
2. From Substance Abuse treatment records.
3. Use or disclosure of your health information for marketing purposes.
4. Disclosures of PHI that are considered a sale.
Exclusive Care will not disclose your health information for marketing, fundraising, or other
reasons not listed above without your prior written permission, and you may withdraw that
permission in writing at any time. If you do, Exclusive Care will no longer use or disclose health
information about you for the reasons you permitted. Exclusive Care is unable to retract
disclosures already made with your permission, and must retain records of care already
provided.
C. Use and Disclosure Requiring an Opportunity for You to Agree or Object
In certain cases, Exclusive Care may use and disclose health information only if it informs you
in advance and provides an opportunity for you to agree or object, as required by state and
federal law:
1. Exclusive Care may include your name, location in the facility, general condition, and
religious affiliation in a facility directory while you are a patient so your family, friends and
clergy can visit you and know how you are doing.
2. To individuals assisting with your treatment or payment.
3. To assist with disaster relief and to notify your family about you.
D. Use and Disclosure NOT Requiring Permission or an Opportunity for You to Agree or
Object
EPO: 2022
56
In specific cases, Exclusive Care may use and disclose the following health information without
your permission and without providing you the opportunity to agree or object:
1. As required by law.
2. For public health activities, which may include the following:
• Preventing or controlling disease, injury or Disability;
• Reporting births and deaths;
• Reporting abuse or neglect of children, elders and dependent adults;
• Reporting reactions to medications or problems with products;
• Notifying people of recalls of products they may use; or,
• Notifying a person exposed to or at risk to contract or spread a disease or
condition.
3. For mandated reporting of abuse, neglect or domestic violence.
4. For health oversight activities necessary for the government to monitor the health care
system government programs and compliance with civil rights laws.
5. To the minimum extent necessary to comply with judicial and administrative proceedings
when compelled by court order, or in response to a subpoena, discovery request or other
lawful process as allowed by law.
6. To law enforcement:
• To identify or locate a suspect, fugitive, material witness, or missing person;
• About the victim of a crime if, under certain limited circumstances, we are unable
to obtain the person’s agreement;
• About a death we believe may be the result of criminal conduct;
• About criminal conduct at the Hospital; or,
• In emergency circumstances to report a crime, the location of a crime or crime
victims, or the identity, description or location of a person who may have committed
a crime.
7. To coroners, medical examiners and funeral directors as necessary for them to carry out
their duties.
8. For organ donation once you are deceased.
9. For public health research in compliance with strict conditions approved and monitored
by an Institutional Review Board.
10. To avert serious threats to the health and safety of you or others.
11. Regarding military personnel for activities deemed necessary by appropriate military
command authorities to assure proper execution of a military mission.

EPO: 2022
57
12. To determine your eligibility for or entitlement to veterans’ benefits.
13. To authorized federal officials for the conduct of lawful intelligence, counter-intelligence,
and other national security activities.
14. To correctional institutions and other law enforcement custodial situations, inmates of
correctional institutions or in custody of a law enforcement official.
15. To determine your eligibility for or enroll you in government health programs.
16. For Workers Compensation or similar programs, to the minimum extent necessary.
E. Rights and Responsibilities
With regard to health information, Exclusive Care recognizes and commits to safeguard your:
1. Right to request restrictions on certain use and disclosure. You have the right to
request restriction or limitation on the health information Exclusive Care uses or
discloses for treatment, payment or health care operations, though the law does not
require Exclusive Care to agree to your request. If Exclusive Care agrees, it will
comply, except to provide Emergency Treatment. Requests must be in writing and
state: the information you want to limit; whether to limit use, disclosure, or both; and
to whom limits apply. For instance, you may ask not to disclose to your spouse.
2. Right to confidential communications. You have the right to ask Exclusive Care to
communicate with you in a certain way, or at a certain location.
3. Right to request to inspect and copy records. You have the right to request to
inspect and obtain copies of your health information including PHI maintained in an
electronic format. If your PHI is available in an electronic format, you may request
electronic access.
Requests may be required in writing, and Exclusive Care may charge you a fee for
the costs of fulfilling your request. This fee is limited to the cost of labor involved in
responding to your request if you requested access to an electronic health record.
Exclusive Care may deny requests to inspect or copy psychotherapy notes, mental
health records, or materials for legal proceedings. You may ask for review of a denial
by another Health Care Professional chosen by Exclusive Care. Exclusive Care will
comply with the results of that review.
4. Right to amend health records. If information Exclusive Care has about you is
incorrect or incomplete, you may ask to amend it. Requests must be in writing, and
provide a reason supporting your request. Exclusive Care may deny your request if it
is not in writing, or does not include a reason supporting it. Exclusive Care may deny
requests if the information:
• Was not created by Exclusive Care;
• Is not health information kept by or for Exclusive Care;
• Is not information you are permitted to inspect and copy; or,
• Is accurate and complete.

EPO: 2022
58
5. Right to an accounting of certain disclosures. You have the right to ask for an
“accounting of disclosures”, including a disclosure involving an electronic health
record. This is a list of disclosures of your PHI that Exclusive Care has made to others,
except those necessary to carry out health care treatment, payment, or operations
(does not include electronic records); disclosures made by you; or in certain other
situations. The first list you request in a twelve-month period is free. Exclusive Care
may charge you the cost of providing or reproducing additional lists. When told the
cost, you may withdraw or modify your request.
6. Right to obtain a paper copy of the notice of privacy practices upon request.
You have a right to a paper copy of this notice, even if you received this notice
previously or agreed to receive this notice electronically.
7. Right to file complaints without fear of retaliation. Under law, you cannot be
penalized for filing a complaint. If you believe Exclusive Care violated your privacy
rights, you may file a complaint with Exclusive Care, the County of Riverside Privacy
Office, or with the U.S. Secretary of Health and Human Services.
Privacy Complaint Contacts
Exclusive Care Plan
P.O. Box 1508
Riverside, CA 92502
(800) 962-1133
County of Riverside
Privacy Office
P.O. Box 1569
Riverside, CA 92502
(951) 955-1000
U.S Department of Health
& Human Services
Region IX Office of Civil
Rights
50 United Nations Plaza,
Room 322
San Francisco, CA 94102
TEL: (415) 437-8310
TDD: (415) 437-8311
FAX: (415) 437-8329
Release Of Information
The Health Insurance Portability and Accountability Act (HIPAA) includes a provision that grants
individuals certain rights regarding their Protected Health Information (PHI) maintained by their
health plan. HIPAA also defines the obligation that the Health Plan has in protecting each
Member’s PHI. Each Member’s PHI will be used and disclosed only in accordance with the Plan’s
privacy policy outlined above and applicable law.
At the time of enrollment, each Member agrees to authorize the Plan, or its designee, to have
access to and use of his/her medical records (including mental health medical records and
medical records for drug and alcohol abuse treatment or prevention) for purposes of utilization
review, quality assurance, surveys, processing of claims, financial audits, ratings, insurance
underwriting, or purposes related to the performance of providing medical care or applying
policies outlined in this Summary Plan Document.
EPO: 2022
59
The Plan continually safeguards PHI. If it is the desire of a Member that the Plan share PHI with
an unknown party or entity not directly involved with a Member’s care, or the administration of
care, please contact the Member Services Department to request a “release of information” form.
Certificate Of Coverage
Upon termination of Plan coverage, a “Certificate of Group Health Plan Coverage” is provided
to you and any affected dependents, which identifies your coverage period with the Plan. The
Plan mails this certificate to your last known address noted in the Plan’s records.
For additional information regarding the Plan’s Privacy Policy Statement and additional copies
of the Plan’s Privacy Policy with respect to medical coverage, contact the Member Services
Department at (800) 962-1133.
SECTION 11: PAYMENT BY THIRD PARTIES
Third Party Recovery Process and Your Responsibilities
If you are ever injured through the actions of another (a third party) and receive compensation
for your medical care, you will be required to reimburse the Plan, or its designee, for the
reasonable value of medical services and benefits provided. The amount of reimbursement shall
not exceed the amount of compensation you receive from the third party.
You must obtain the Plan’s written consent prior to settling any claim or releasing any third party
from liability, if such a release would limit the Plan’s right to reimbursement.
• Should you settle your claim against a third party and compromise the Plan’s
reimbursement rights, the Plan reserves the right to initiate legal action. Attorney fees will
be awarded to the prevailing party.
• The Plan shall be entitled to the payment and reimbursement as provided in this Section
11 regardless of whether the total amount of the recovery of the Member (or his or her
estate, parent or legal guardian) on account of the injury is less than the actual loss
suffered by the Member (or his or her estate, parent or legal guardian). The proceeds of
any judgment or settlement obtained by the Plan (or its designee) or the Member (or his
or her estate, parent or legal guardian) on account of the injury shall first be applied to
satisfy Plan's (or its designee's) claims, liens, and other rights under this Section 11.
You are required to cooperate in protecting the interest of the Plan by providing the Plan with all
liens, assignments and/or other documents. Failure to cooperate with the Plan in this regard
could result in termination of coverage.
Non-Duplication of Benefits with Automobile, Accident or Liability Coverage
If you are receiving benefits as a result of other automobile, accident or liability coverage, the
Plan will not duplicate those benefits. It is your responsibility to take whatever actions are
necessary to receive payment under the other coverage.
Non-Duplication of Benefits with other Group Health Coverage

EPO: 2022
60
• Benefits for Non-Medicare Eligible Members. The Plan provides Benefits up to the
Plan’s reimbursement level when combined with benefit payments you receive from other
group health coverage(s) you or your enrolled dependents may have. If you have other
group health coverage(s), this “Non-Duplication of Benefits” provision may result in
reduced Benefits by the Plan. If Exclusive Care’s EPO or Out-of-Area Benefits are
secondary, and another plan covering you or an Eligible Dependent is the primary plan,
Exclusive Care may not pay any Benefits if the primary plan's benefits are equal to or
greater than Exclusive Care's Benefits. The goal of the “Non-Duplication of Benefits” rule
is to maximize coverage for expenses, and to prevent any payment duplication.
• The Plan determines Benefits in accordance with the National Association of Insurance
Commissioners’ guidelines, and California law.
• In order to ensure proper coordination with other health coverage(s) you may have, you
must inform the Plan of any other health coverage for which you or your enrolled
dependents may be eligible.
• If the Plan pays more Benefits than are appropriate, the Plan may recover excess
payments from you, the plan with primary responsibility, or any other person or entity that
benefited from the overpayment.
Order of Benefit Determination
The rules establishing the order of benefit determination are:
1. The benefits of a plan which covers the Member as an active employee will be determined
before the benefits of a plan which covers the Member as a non-active employee (i.e., a
retired or laid off employee, a COBRA participant, etc.), or as a dependent. If the other
plan does not have this rule, and if as a result the plans do not agree on the order of
benefit determination, the rule of the other plan will prevail;
2. When the Member is a dependent child and such child’s parents are not separated or
divorced, the benefits of the plan of the parent whose birthday falls earlier in the year are
determined before those of the plan of the parent whose birthday falls later in the year,
however;:
• If both parents have the same birthday, the benefits of the plan which covered the
parent longer are determined before those of the plan which covered the other
parent for a shorter period of time; or
• If the other plan does not have this rule, and if as a result the plans do not agree
on the order of benefit determination, the rule of the other plan will prevail.
When the Member is a dependent child whose father and mother are legally separated or
divorced:
1. The benefits of the plan which covers the Member as a dependent child of the parent with
custody will be determined first, except that if a court decree assigns financial
responsibility for the health care coverage of a dependent child to one of the parents, the
benefits of the assigned parent’s plan will be determined first and the other parent’s plan
will be determined second;
2. The plan of the spouse of the parent with custody will be determined next;

EPO: 2022
61
3. The plan of the parent not having custody of the child will be determined last.
If none of the above rules establish an order of benefits determination, the benefits of the plan
which has covered the Member for the longer period of time are determined before those of the
plan which has covered the Member for the shorter period of time.
When this provision operates to reduce the total benefit otherwise payable to a person covered
under the Plan during any claim determination period, each Benefit will be reduced
proportionately, and such reduced amount will be charged against any applicable Benefit limit
of the Plan.
Workers’ Compensation
If you are receiving benefits as a result of a work-related injury or illness the Plan will not
duplicate those benefits.
It is your responsibility to take whatever action is necessary to receive payment under workers’
compensation laws, when such payments can reasonably be expected.
If for whatever reason, the Plan duplicates benefits to which you are entitled under workers’
compensation law, you are required to reimburse the Plan at prevailing rates, immediately after
receiving the monetary award, whether by settlement or judgment.
In the event of a dispute arising between you and the workers’ compensation administrator, the
Plan will provide the Benefits described in this SPD until the dispute is resolved.
If you receive a workers’ compensation benefit which includes payment of future medical costs,
you may be liable for reimbursing the Plan.
SECTION 12: HEALTH PLAN ADMINISTRATION AND INTERPRETATION
Funding of Benefits and Administration
The Plan is self-insured and unfunded. In other words, the Plan is funded through premium
contributions made by Members and participating employer groups, and all Benefits are paid
from Plan assets which are maintained by the County of Riverside. The Plan Administrator may
also establish a trust for the payment of Benefits.
Your rights to Benefits under the Plan shall be determined in accordance with the terms of the
Plan as provided in this Summary Plan Document. Furthermore, the County has complete and
discretionary authority to determine all questions relating to the interpretation of ambiguous,
unclear or implied terms in this Summary Plan Document, to make any findings of fact or law
needed to determine eligibility to participate in the Plan, and to receive Benefits. The County
also has the full responsibility and authority to take any and all actions not specifically described
in this Summary Plan Document that may be necessary or appropriate for the effective
administration of the Plan. The decisions of the Plan Administrator and its representatives shall
be given the maximum deference permitted by law.
The County of Riverside refrains from any conduct that constitutes fraud and dishonest dealing
or unfair competition, as defined by Section 17200 of the Business and Profession Code.

EPO: 2022
62
Members may file a complaint with the State of California Department of Managed Health Care
regarding violations of Section 17200 of the Business and Profession Code.
All changes to Benefits, Participating Providers, and health care services provided under
the Plan will be ultimately determined by the County of Riverside’s Board of Supervisors,
in conjunction with the County of Riverside Human Resources Department.
SECTION 13: DEFINITION OF TERMS
Acute Condition - Care provided in the course of treating an illness, injury or condition marked
by a sudden onset or change of status requiring prompt attention, which may include
hospitalization, but which is of limited duration and not expected to last indefinitely.
Administrative Review Committee - As part of the Member Grievance Procedure, the
committee of individuals selected to provide a secondary review of a Member’s appeal upon
receipt of an initial pre-authorization/claim denial notice.
Allowed Charges - An amount on which the Plan’s payment/reimbursement for a Covered
Service is based; an amount which is consistent with the current rate or charge, in a certain
geographical area, for identical or similar services, as determined by the Plan.
Ambulatory Surgical Center - A facility that performs surgery on a non-hospitalized patient.
The patient returns home the same day the surgery is performed.
Billed Charges - The amount the provider actually charges for services provided to a Member.
Behavioral Health/Behavioral Health Service - Services rendered or made available to a
Member for treatment of Mental Health and Substance Abuse Disorders.
Benefits - Covered Services paid by the Plan subject to all other terms and conditions of the
Summary Plan Document.
Brand Name Drug - A Brand Name Drug is a drug marketed under a proprietary trademark
protected name.
Calendar Year - The period of time commencing at 12:01 a.m. on January 1 and ending at 12:01
a.m. on the nest January 1. Each succeeding like period will be considered a new Calendar Year.
A Calendar Year is necessary for purposes of determining the number of treatment days for the
maximum benefit specified for each benefit under the Plan.
Chiropractic Care - Chiropractic services billed by any participating, licensed provider which
will apply toward the chiropractic benefit Calendar Year maximum.
Chronic Condition - Treatment for an illness, injury or condition which does not require
hospitalization (although confinement in a lesser facility may be appropriate), which may be
expected to be of long duration, has no reasonably predictable date of termination, and may be
marked by recurrence requiring continuous or periodic care as necessary.
EPO: 2022
63
Clinical Necessity/Clinically Necessary - Behavioral Health Services or supplies for treatment
of an active Mental Health or Substance Abuse Disorder which have been established in
accordance with generally accepted professional standards and the Plan’s Utilization Review
Committee to be:
• Rendered for the treatment and diagnosis of a Mental Health or Substance Abuse
disorder as defined by the DSM-IV and limited to impairment of a Member’s mental,
emotional or behavioral functioning;
• Appropriate for the severity of symptoms, consistent with diagnosis, and otherwise in
accordance with generally accepted mental health practice and professionally recognized
standards;
• Not furnished primarily for the convenience of the Member, the attending Participating
Practitioner, or other provider of service;
• Furnished at the most appropriate level which may be provided safely and effectively to
the Member.
Coinsurance – The Member’s share of the cost of Covered Services.
Copay - The Member’s share of the costs to be paid at the time Covered Services are received.
Covered Expense(s) – Any Medically Necessary expense incurred by a Member subject to all
other terms and conditions of the Summary Plan Document
Covered Service(s) - Any Medically Necessary service received by a Member subject to all
other terms and conditions of the Summary Plan Document
Cost of Coverage - You are responsible for the payment of the entire premium for coverage for
yourself and your covered Eligible Dependents.
Custodial Care - Care provided primarily for the maintenance of the patient or which is designed
to provide room and board or meet the activities of daily living (which may include nursing care,
training in personal hygiene and other forms of self care); or care furnished to a Member who is
mentally or physically disabled, and who is not under specific medical, surgical or psychiatric
treatment to reduce the Disability to the extent necessary to enable the patient to live outside an
institution providing such care or when, despite such treatment, there is no reasonable likelihood
that the Disability will be so reduced.
Day Treatment Center - A facility which provides Mental Health and/or Substance Abuse
Services on a full or part-day basis pursuant to a written Treatment Plan approved and monitored
by the Plan, and which facility is also licensed, certified or approved as such by the appropriate
state agency.
Deductible - The Deductible is the portion of medical expenses you must pay each Calendar
Year before the Plan will pay Benefits.
EPO: 2022
64
Dental Care - Services or treatment on or to the teeth or gums whether or not caused by
accidental injury, including any appliance or device applied to the teeth or gums.
Disability - An injury, an illness (including any Mental Health or Substance Abuse Disorders),
or a condition (including pregnancy); however,
• All injuries sustained in any one accident will be considered one Disability;
• All illnesses existing simultaneously which are due to the same or related causes will be
considered one Disability;
• If any illness is due to causes that are the same as, or related to, the causes of any prior
illness, the succeeding illness will be considered a continuation of the previous Disability
and not a separate Disability.
Domestic Partner - An individual, with whom the Member has registered as a domestic partnership
with the State of California, as evidenced by a signed California Declaration of Domestic Partnership.
Such individual must live in a mutually exclusive relationship with the Member, both must be jointly
responsible for each other’s welfare and financial obligations, and live in the same principal
residence and intend to do so indefinitely. In addition, a domestic partnership must consist of two
individuals who are at least 18 years of age and are of either the same-sex or, of the opposite sex
as long as one individual is over the age of 62. Individuals in a domestic partnership also must be
unmarried and not be blood relatives close enough to bar marriage in the State of California.
Drug Formulary/Formulary - A listing of drugs in major therapeutic categories, selected by an
independent committee of medical and pharmacy professionals who are either Physicians or
clinical pharmacists with a doctorate in pharmacology (Pharm D), and which are considered to
be preferred over other drug alternatives. Formulary drugs are evaluated for: (1) indications; (2)
side effects; (3) interaction with other drugs; (4) dosage form availability; (5) pharmacokinetics
(how a drug is absorbed, distributed, metabolized and excreted); and (6) Physician preference.
The objective of the Formulary is to improve the quality of patient care by promoting high quality,
cost-effective prescribing and dispensing of prescription drugs to meet Members’ prescription
drug needs.
DSM-IV - The Diagnostic and Statistical Manual of Mental Disorders (most current edition) which
lists diagnostic criteria for Mental Health Disorders as defined by the American Psychiatric
Association.
Durable Medical Equipment - Equipment intended for repeated use, which is primarily and
customarily used to serve a medical purpose, and generally is not useful to a person in the
absence of an illness or injury. Items considered “Other Medical Equipment” is defined in a
separate entry in the Definition of Terms.
Eligible Child(ren) - Dependent natural children, adopted children, foster children,
grandchildren, and stepchildren under your employer group’s limiting age; any child, who is
under your employer group’s limiting age, for whom you have legal custody, have been required
to cover under your medical plan as part of a QMCSO or who resides with you (generally in the
absence of the natural or adoptive parent) and who is economically dependent upon you; or an
otherwise Eligible Child past your employer group’s limiting age if the child is incapable of self-
EPO: 2022
65
support because of a mental or physical handicap and you continue to claim the child as a
dependent on your federal income tax return.
Eligible Dependent (s) - A legal spouse or Domestic Partner, and all Eligible Child (ren).
Eligible Spouse – A legal spouse or Domestic Partner as defined by California Law.
Emergency Care - Care rendered in response to the sudden and unexpected onset of acute
illness or accidental injury requiring alleviation of severe pain; or immediate medical or surgical
care which you secure immediately after the onset, or as soon thereafter as practicable, but in
no event later than 24 hours after onset. The absence of immediate medical attention could
reasonably be expected to result in any of the following:
• Placing the Member’s health in serious jeopardy;
• Serious impairment to bodily functions; or
• Serious dysfunction of any bodily organ or part.
Emergency Condition - A Mental Health/Substance Abuse Disorder which manifests itself by
acute symptoms of sufficient severity such that the absence of immediate Behavioral Health
Services could reasonably be expected to result in the following:
• immediate harm to self or others;
• placing the Member’s health in serious jeopardy;
• serious impairment of the Member’s functioning; or
• serious and permanent dysfunction of the Member.
Emergency Treatment - The immediate and unscheduled screening, examination, and
evaluation of a Member by a Participating Practitioner at a Participating Facility to determine if
an Emergency Condition exists. If an Emergency Condition is found to exist, Emergency
Treatment will include the care and treatment by the Participating Practitioner and Participating
Facility necessary to relieve or eliminate the Emergency Condition, within the capacity of the
Participating Facility.
Exclusive Care - The County of Riverside Exclusive Provider Organization (EPO) Health Plan.
Experimental or Investigational - Any treatment, therapy, procedure, drug or drug usage,
facility or facility usage, equipment or equipment usage, device or device usage, or supplies
which are not recognized as being in accordance with generally accepted professional medical
standards, or if safety and efficacy have not been determined for use in the treatment of a
particular illness, injury or medical condition for which it is recommended or prescribed (see
pages 26-27).
FDA - Food and Drug Administration.
Generic Drugs - A Generic Drug available in the marketplace after the Brand Name Drug loses
patent protection; contains a medication’s basic chemical components and usually has a Brand
Name Drug equivalent. The FDA requires that Generic Drugs have the same form as their Brand
Name Drug equivalents. Generic Drugs must meet the same FDA standards as Brand Name
EPO: 2022
66
Drugs and are tested and certified by the FDA to be as effective as their Brand Name Drug
equivalents.
Health Plan - The plan(s) as described in this Summary Plan Document, as applicable.
Health Care Professional – Dentist, optometrist; podiatrist or chiropodist; clinical psychologist;
chiropractor; acupuncturist; licensed clinical social worker; licensed professional clinical
counselor; marriage, family and child counselor; physical therapist; speech pathologist;
audiologist; radiologist; licensed occupational therapist; physician assistant; registered nurse;
registered dietitian for the provision of diabetic medical nutrition therapy only; a nurse practitioner
and /or nurse midwife providing services within the scope of practice as defined by the
appropriate clinical license and/ or regulatory board.
Home Health - Home Health care providers who are licensed according to state and local laws
to provide skilled nursing and other services on a visiting basis in your home and recognized as
Home Health providers under Medicare.
Hospice - A program designed to care for the terminally ill individual with a life expectancy
of six (6) months or less. Hospice programs include the following components for individuals
who have decided to no longer pursue curative medical treatment:
Control of pain and other symptoms through medication, environmental adjustment,
and education;
Psychosocial support for both the patient and family, including all phases from
diagnosis through bereavement;
Medical services equal with the needs of the patient;
Interdisciplinary "team" approach to patient care, patient and family support, and
education under physician leadership; and
Specially trained personnel with expertise in care of the dying and their families.
Hospital - An institution which is licensed under all applicable state and local laws and
regulations to provide, under supervision of Physicians, diagnostic and therapeutic services for
the medical diagnosis, treatment and care of the injured, disabled or sick persons in need of
acute Inpatient medical and psychiatric or psychological care, and which is registered as a
general Hospital with the American Hospital Association and accredited by the Joint Commission
on Accreditation of Healthcare Organizations. Hospital also includes:
• A psychiatric Hospital licensed as a health facility accredited by the Joint Commission on
Accreditation of Health Care Organizations; or
• A licensed health facility operated primarily for the treatment of alcoholism and/or
substance abuse accredited by the Joint Commission on Accreditation of Health Care
Organizations; or
• A “psychiatric health facility” as defined in Section 1250.2 of the Health and Safety code.
Infertility - Either (1) the presence of a demonstrated bodily malfunction recognized by a licensed
Doctor of Medicine as a cause of Infertility or (2) because of a demonstrated bodily malfunction,
EPO: 2022
67
the inability to conceive a pregnancy or to carry a pregnancy to a live birth after a year or more
of regular sexual relations without contraception.
Inpatient - An individual confined as a bed patient in a Hospital or Skilled Nursing Facility who
requires routine or specialized Hospital services. Also refers to services rendered in Hospital or
Skilled Nursing Facility while confined as a bed patient.
Medical Director - A Physician, designated by the Plan, who is responsible for the
medical/clinical administration of the Plan.
Medical Group - A group of Physicians practicing in a professional corporation or association
which has entered into a written agreement with the Plan to provide Covered Services to
Members.
Medical Management Unit - The Plan’s Medical Director and qualified clinical/case
management staff under his/her direction, who provide pre-authorization review, Medical
Necessity review, and other medical review/case management activities, to assist in the
administration and determination of Covered Services and Benefits.
Medically Necessary/Medical Necessity – Drugs, devices, procedures, treatments, services
or supplies provided by a provider facility or individual provider which are required for treatment
of an Exclusive Care member’s illness, injury, diseased condition or impairment and are:
• Consistent with the symptoms or diagnosis and the member is an appropriate candidate
for the proposed treatment; and
• Appropriate treatment, according to generally accepted standards of medical practice;
and
• Not furnished primarily for the convenience of the patient, the attending Physician or
another provider; and
• Not considered investigational or experimental, or
• Not excessive in scope, duration, or intensity to provide safe, adequate and appropriate
treatment. Any service or supply provided at a facility will not be considered medically
necessary if the symptoms or condition indicate that it would be safe to provide the service
or supply in a less comprehensive setting.
The fact that any particular provider individual may prescribe, order, recommend or approve a
service, supply or level of care does not, of itself, make such treatment medically necessary or
make the charge a Covered Expense.
Medicare - The programs of medical care coverage set forth in Title XVIII of the Social Security
Act, as amended by Public Law 89-97, or as thereafter amended.
Member - An employee, retiree, Eligible Spouse, Eligible Child(ren) or Eligible Dependent
enrolled in the Plan. Also referred to as “you” or “your”.
Mental Health Disorder(s) - A mental disorder diagnosed by a licensed qualified Participating
Practitioner according to the criteria in the DSM-IV and limited to impairment of a Member’s
mental, emotional or behavioral functioning on a daily basis.
EPO: 2022
68
Mental Health Services - Psychoanalysis, psychotherapy, counseling, medical management or
other services most commonly provided by a psychiatrist, psychologist, licensed clinical social
worker, or marriage/family/child counselor, for diagnosis or treatment of mental or emotional
disorders or the mental or emotional problems associated with illness, injury, or any other
condition.
Network - The Hospitals, Medical Groups, Physicians, Specialists, clinics, pharmacies and other
individual health care providers contracting with Exclusive Care to provide its Members with
treatment and services.
Non-Formulary Drugs – Outpatient Generic and Brand Name Drugs that are not included in
the Drug Formulary. These drugs are covered under the Plan but require a higher Member
Copay. Most non-preferred drugs have a more cost-effective alternative on the Preferred Drug
List.
Occupational Therapy - Treatment under the direction of a Physician and provided by a certified
occupational therapist, utilizing specific training in daily living skills, to improve and maintain a
patient’s ability to function.
Orthotics - An orthopedic appliance or apparatus used to support, align, prevent or correct
deformities or to improve the function of movable body parts.
Other Medical Equipment - Corrective appliances, artificial aids, prosthetics and orthotics that
are part of a corrective appliance, therapeutic footwear (limits may apply), urinary catheters
(covered for a Member who has permanent urinary incontinence or permanent urinary
retention).
Outpatient - An individual receiving services under the direction of a Health Plan provider, but
not as an Inpatient.
Participating Chiropractor/ Hospital/ Physician/ Provider - An independent provider who has
a contractual agreement with Exclusive Care to provide Covered Services to Members.
Participating Facility - A facility that is under contract with Exclusive Care to provide Inpatient,
residential, day treatment, partial hospitalization, or Outpatient care for the diagnosis and/or
treatment of Mental Health Disorders or Substance Abuse Disorders.
Participating Mental Health/Substance Abuse Provider - A Participating Facility or
Participating Practitioner who provides Mental Health Services.
Participating Pharmacy – A retail pharmacy contracted by Exclusive Care’s Pharmacy
Benefits Manager to provide Members with outpatient prescription drug services.
Participating Practitioner - Any licensed qualified Health Care Professional who has entered
into a contractual agreement with Exclusive Care to provide Behavioral Health Services.
EPO: 2022
69
Pharmacy and Therapeutic Committee - A committee of practicing Physicians and
pharmacists who are responsible for creating and updating the Drug Formulary.
Pharmacy Benefit Manager – The provider organization that has contracted with Exclusive
Care to provide access to a network of retail pharmacies and pharmacy benefit management
services including Formulary maintenance.
Physical Therapy - Treatment under the direction of a Physician and provided by a registered
physical therapist, certified occupational therapist or licensed doctor of podiatric medicine,
utilizing physical agents, such as ultrasound, heat and massage, to improve a patient’s
musculoskeletal, neuromuscular and respiratory systems.
Physician - An individual licensed and authorized to engage in the practice of medicine (M.D.)
or osteopathy (D.O.);
Physician Review Committee – A committee appointed by Exclusive Care to review a
Member’s appeal of a pre-authorization or claim denial, upon the request of the Member.
Plan - Exclusive Care Exclusive Provider Organization (EPO) providing Benefits for Covered
Services subject to all other terms and provisions of the Summary Plan Document.
Plan Service Area - The County of Riverside and such adjacent communities as are designated
by Exclusive Care.
Primary Care Provider - A general practitioner, board-certified or eligible family practitioner,
internist, or pediatrician who has contracted with the Plan to provide primary care services to
Members and to refer, authorize, supervise and coordinate the provision of all Benefits to
Members in accordance with the Plan’s provisions.
Prosthetics – Devices (other than dental) which replace all or part of an internal body organ
(including contiguous tissue), or replace all or part of the function of a permanently inoperative
or malfunctioning internal body organ.
Psychiatric Admission - The scheduled and unscheduled admission of a Member by a
Participating Practitioner to a Participating Facility for care and treatment Clinically Necessary
to relieve or eliminate the Emergency Condition due to a Mental Health/Substance Abuse
Disorder which manifests itself by acute symptoms of sufficient severity such that the absence
of immediate Behavioral Health Services could reasonably be expected to result in the following:
(i) immediate harm to self or others; (ii) placing the Member’s health in serious jeopardy; (iii)
serious impairment of the Member’s functioning; or (iv) serious and permanent dysfunction of
the Member.
Qualified Public Employer Group
EPO: 2022
70
The employees, retirees, and the dependents of those employees and retirees, of any city,
county, city and county, public entity, or political subdivision that has signed a participating
health care service agreement with Exclusive Care. Exclusive Care is not available to the
general public pursuant to Section 1349.2 of the California Health and Safety Code.
QMCSO - A Qualified Medical Child Support Order, as defined in Section 609 of the Employment
Retirement Income Security Act of 1974, as amended.
Rehabilitation - Care furnished primarily to restore an individual’s ability to function as normal as
possible after a disabling illness or injury. Rehabilitation services may consist of the combined use
of medical, social, educational, occupational, or vocational treatment modalities and are provided
with the expectation that the patient has restoration potential and will realize significant improvement
in a reasonable length of time.
Residential Treatment Center - An acute care facility which provides Mental Health and
Substance Abuse services in an acute, Inpatient setting, pursuant to a written Treatment Plan
approved and monitored by a Physician and which facility also:
• Provides 24-hour nursing and medical supervision; and
• Is licensed, certified or approved as such by the appropriate state agency.
Residential Treatment Facility - A facility which provides Substance Abuse services in a
residential setting on a full- or part-day basis, pursuant to a written Treatment Plan approved
and monitored by the Plan, and which is licensed, certified or approved as such by the
appropriate state agency.
Respiratory Therapy - Treatment under the direction of a Physician and provided by a trained
and certified respiratory therapist, to preserve or improve a patient’s pulmonary function.
Respite Care – Continuous care of the patient in the most appropriate setting for the primary
purpose of providing temporary relief to the family from the duties of caring for the patient.
Schedule Of Benefits - A summary of the Covered Services/Benefits provided by the Plan, the
amount that the Plan will pay towards the cost, and the Copay and other amounts, if any, that
the Member pays towards the cost.
Severe Mental Illness – A Severe Mental Illness is defined as one or more of the following
conditions: schizophrenia, schizoaffective disorder, bipolar disorder (manic depressive illness),
major depressive disorders, panic disorder, obsessive-compulsive disorder, pervasive
developmental disorder or autism, anorexia nervosa, and bulimia nervosa.
Skilled Nursing Facility - A facility licensed by the California State Department of Health as a
“skilled nursing facility” or any similar institution licensed under the laws of any other state,
territory, or foreign country.
Specialist - Any duly licensed Physician, osteopath, psychologist or other Practitioner (as
EPO: 2022
71
defined by Medicare) who provides health care services for a specific disease or body part and
to whom your Primary Care Provider may refer you. Also, any duly licensed emergency room
Physician who provides Emergency Care services to you.
Speech Therapy - Treatment under the direction of a Physician and provided by a licensed
speech pathologist or speech therapist, to improve or retrain a patient’s vocal skills.
Substance Abuse/Substance Abuse Disorder - An addictive relationship between a Member
or his/her Eligible Dependent, and any drug, alcohol, or chemical substance that can be
documented according to the criteria in the DSM-IV. Substance Abuse does not include
addiction to or dependency on:
• Tobacco in any form; or
• Food substances in any form.
Summary Plan Document (SPD) - The written evidence of coverage furnished to Members of
the Health Plan, providing details of Benefits and Covered Services under the Health Plan.
Treatment Plan – Services or a plan of treatment preauthorized by the Plan during a contract
period that must be commenced during the same contract period. To qualify for continuing
treatment in a subsequent contract period, the services or plan of treatment must be
reauthorized. Otherwise, only the Benefits in effect during a contract period are available or
covered.
Urgent Care/Urgently Needed Services – Urgent Care or Urgently Needed Services are
Medically Necessary services required after regular business hours to prevent serious
deterioration of your health resulting from unforeseen illness or injury manifesting itself by
acute symptoms of sufficient severity which may include severe pain, such that the treatment
can not be delayed until your Primary Care Provider is available;
Urgent Care or Urgently Needed Services are provided for less serious medical conditions than
Emergency Care Services, such as:
Non life-threatening cuts which nevertheless require immediate suturing to ensure proper
healing;
Acute illnesses where a delay in care would result in a serious deterioration in your health;
Utilization Review Committee – The Medical Management Utilization Review Committee which
meets periodically and consists of the Medical Director, licensed Physicians and other case
management staff.
72
HEALTH PLAN ADDRESSES AND
IMPORTANT TELEPHONE NUMBERS
Member Services Department:
EXCLUSIVE CARE Member Services
P.O. Box 1508
Riverside, CA 92502-1508
(800) 962-1133, press option 1
8:00 a.m. – 5:00 p.m. Monday – Friday
Email: epo@rivco.org
Claims Department:
EXCLUSIVE CARE Claims
P.O. Box 1508
Riverside, CA 92502-1508
(800) 962-1133, press option 2
8:00 a.m. - 5:00 p.m. Monday – Friday
Mental Health/Substance Abuse Services:
EXCLUSIVE CARE Medical Management
P.O. Box 1508
Riverside, CA 92502-1508
(800) 962-1133, press option 3
8:00 a.m. - 5:00 p.m. Monday – Friday

73
