LIFEPAK
®
20e
defibrillator/monitor
Instructor guide

Contents
How to use this guide ...................................................................................................1
Training tips .....................................................................................................................1
AED training course ......................................................................................................3
Learning objectives ..........................................................................................................3
Equipment and materials .................................................................................................3
LIFEPAK 20e debrillator/monitor AED training class ..................................................3
Early debrillation ........................................................................................................ 4
Biphasic energy ...............................................................................................................4
Controls and features ...................................................................................................5
Device maintenance ...................................................................................................... 6
AED operation..................................................................................................................8
Manual training course .............................................................................................11
Learning objectives ........................................................................................................11
Equipment and materials ...............................................................................................11
LIFEPAK 20e debrillator/monitor Manual User Training Class .................................12
Early debrillation ...................................................................................................... 12
Biphasic energy .............................................................................................................13
Controls and features .................................................................................................13
Additional areas not shown ...........................................................................................21
Device maintenance .................................................................................................... 22
Manual debrillation .................................................................................................24
Synchronized cardioversion procedure ..............................................................26
Noninvasive pacing .....................................................................................................28
ECG monitoring ............................................................................................................. 31
Optional feature: Pulse oximetry ..........................................................................33
Optional feature: EtCO
2
.............................................................................................34
Data management ........................................................................................................35
Other functions .............................................................................................................37
Instructor guide | 1
How to use this guide
The LIFEPAK 20e debrillator/monitor is easy to use and enables clinicians at every
level to focus on the most important task at hand—saving a patient’s life. The
LIFEPAK 20e debrillator/monitor is highly intuitive to use, and adapts to various
patient environments. With this comprehensive guide, you’ll be able to train your
staff to effectively use the device.
This instructor guide is an introduction to the basic operation of the LIFEPAK 20e
debrillator/monitor. It does not suggest protocols or policies regarding the use of
the debrillator. Refer to Operating Instructions for complete directions for
use, indications, contraindications, warnings, precautions, and potential
adverse events.
This guide is designed for use with the factory default conguration of the LIFEPAK 20e
debrillator/monitor, which is compliant with the 2015 American Heart Association
Guidelines. It is important to be familiar with the conguration of your particular
debrillator. Moving, removing, highlighting, and adding content to this outline to meet
individual user needs is encouraged. Hands-on practice and application with scenarios
promote learning retention.
Training tips
This guide is divided into four sections:
AED operation
Manual operation
Optional features
Data management and other functions
The AED mode is easy for healthcare professionals of all skill levels to quickly understand
and use. This training course reviews the basic operation of the LIFEPAK 20e debrillator/
monitor in AED mode. The manual mode operation is for the ALS providers and reviews
the manual operation and functions of the LIFEPAK 20e debrillator/monitor.
The LIFEPAK 20e debrillator/monitor retains data for two or more patients when
you switch the power off or remove the batteries. The device automatically stores a
CODE SUMMARY™ report as part of the patient report for each patient. This section
describes how to access this information and other functions associated with the
LIFEPAK 20e debrillator/monitor.
All sections are optimally taught in a hands-on format. Instructors should rst demonstrate
how to use the debrillator and then have students practice. Ideally, students will receive
enough practice and coaching from the instructor to ensure they can use the device with
condence in an actual emergency.
Back to contents
Instructor guide | 3
AED training course
The AED mode is highly intuitive and easy for healthcare professionals of all skill levels
to quickly understand and use. This training course reviews the basic operation of the
LIFEPAK 20e debrillator/monitor in AED mode.
Learning objectives
The overall objective of this inservice is to provide an overview of the basic steps of
operation of the identied controls, indicators, and connectors of the LIFEPAK 20e
debrillator/monitor. Upon completion of this course, participants will be able to:
• Verbalize the importance of early debrillation.
• Locate and identify the debrillator’s front panel controls, indicators and connectors.
• Demonstrate QUIK-COMBO
®
electrode application.
• Demonstrate steps for automated external debrillation (AED).
• Demonstrate the paper change.
• Demonstrate routine daily testing.
Equipment and materials
The following is a list of accessories and support material recommended for training on
the LIFEPAK 20e debrillator/monitor. It is essential that all equipment be inspected
and tested to ensure proper function prior to training according to the Basic Orientation
section of the Operating Instructions.
Equipment
• LIFEPAK 20e debrillator/monitor
Accessories
• QUIK-COMBO therapy cable
• Test plug
• EDGE System™ electrodes with QUIK-COMBO connector
(or clip-on training electrodes)
• 3-lead or 12-lead patient simulator
• AC power cord
• 50 mm ECG printer paper
Support materials
• Quick Reference Cards
• Student Study Guide
• Operating Instructions
• Performance Evaluations
LIFEPAK 20e debrillator/monitor AED training class
The following lists the content that should be covered during a typical
AED Operation Training Class.
• Early Debrillation
• Biphasic Technology
• Controls and Features
• AED Operation
• Device Maintenance
Back to contents
4 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Early defibrillation
A New England Journal of Medicine study of 6,789 in-hospital cardiac arrest events due
to ventricular brillation or pulseless ventricular tachycardia reported 70% received
debrillation in 2 or less minutes from recognition of Cardiac Arrest (CA). The survival
rate (signicantly) declined for the 30% of the patients who received debrillation more
than two minutes after cardiac arrest.
1
The American Heart Association (AHA) Guidelines for cardiopulmonary resuscitation
recommended debrillation within 2 minutes of collapse in the hospital setting. The
AHA suggests hospitals deploy AEDs throughout the hospital to achieve the target time
and train staff to use the AEDs.
AEDs can help your hospital staff improve their ability to deliver the rst shock within
the recommended 2 minute guidelines. The LIFEPAK 20e debrillator/monitor can be
used in AED mode to debrillate without having to learn ECG interpretation. The AED is
simple to use because it is designed to automatically analyze the patient’s heart rhythm
and advise you which steps to take. In AED mode the device automatically selects the
appropriate energy dosing.
Biphasic energy
Health care providers may be confused about the right energy dose for biphasic
waveforms because different debrillator manufacturers recommend different energy
dosing protocols. It is important to clarify the correct recommended energy dose for
biphasic waveforms in order to avoid possible confusion that may result in a delay of
therapy. ADAPTIV biphasic technology provides the option to escalate to 360J for best
results. Studies show that rebrillation is common among ventricular brillation (VF)
CA patients and that debrillation of recurring episodes of VF is increasingly difcult.
2,3,4
LIFEPAK devices give you the option to escalate your energy dosing up to 360J for
difcult to debrillate patients.
Fortunately, all AEDs are programmed to follow a predened energy dosing protocol.
In other words, the healthcare provider doesn’t have to worry about energy dosing.
The AED performs this automatically.
A biphasic waveform sends current one way at the start of the shock and then reverses
it so the current ows in the opposite direction. A biphasic shock is a gentler but more
effective shock. Stryker recommends a dosing protocol of 200-300-360 joules and is
the factory default setting in all LIFEPAK debrillators. Stryker believes this energy
protocol can help minimize unnecessary CPR interruptions that result from ineffective
debrillation shocks.
Back to contents
Instructor guide | 5
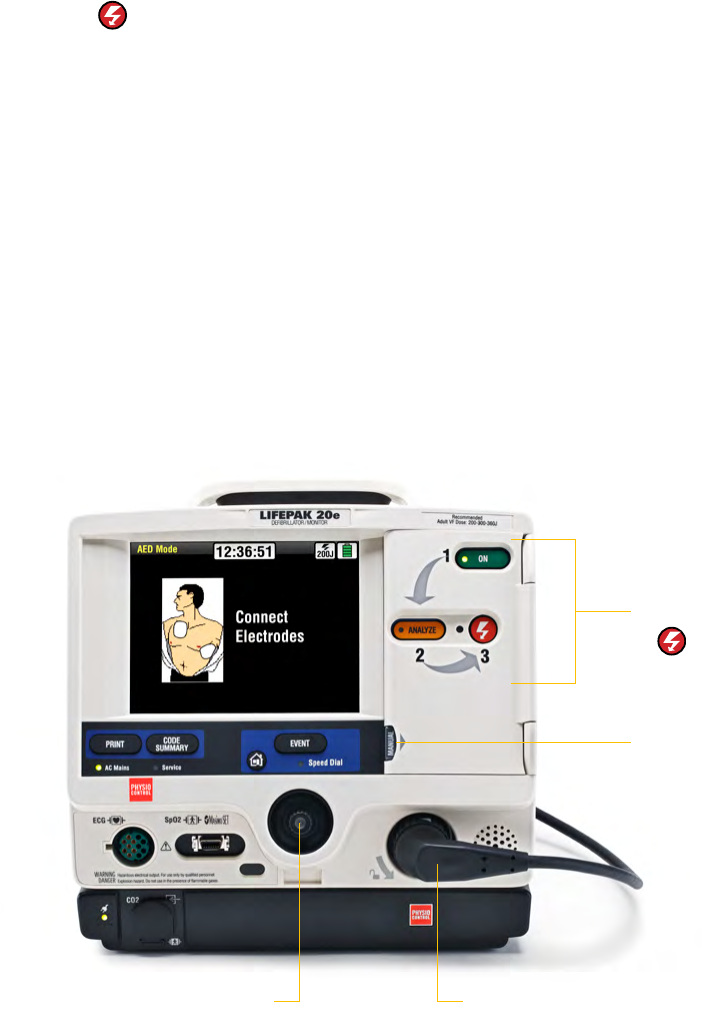
Controls and features
In this section, the goal is to point out the different buttons and physical features pertinent
to an AED user. Each of these features will be reviewed in greater detail later in this guide.
Refer to the Operating Instructions for additional information.
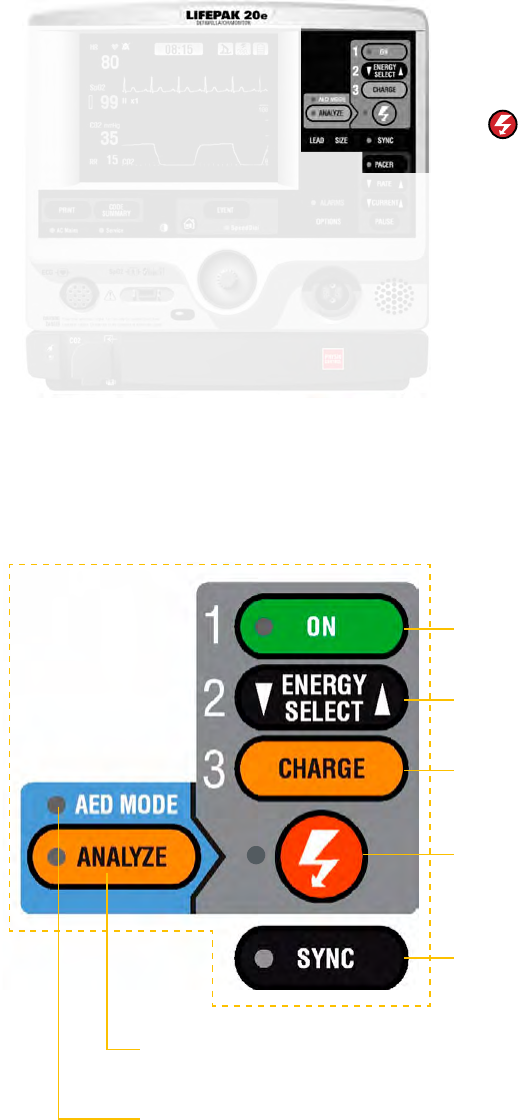
AED buttons
Three buttons used for AED operation.
1. ON
2. ANALYZE
3.
(SHOCK)
Speed dial
Scrolls through and selects menu items.
Therapy cable connector
Connects therapy cable to the device
Manual button
Used to enter Manual Mode; pressing it opens the door and automatically takes the
LIFEPAK 20e debrillator/monitor out of AED mode and puts it into Manual Mode.
*Note: If the debrillator is in AED mode and the door is open, or off, press
ENERGY SELECT once to enter Manual Mode. Full manual mode description is
included in the Manual Mode Training Course for ALS providers.
Therapy cable (not shown)
The therapy cable is a debrillation cable that attaches to therapy electrodes and to the
test plug. The LIFEPAK 20e debrillator/monitor should be stored with the therapy cable
plugged into the lower right hand side of the device.
AED buttons
1. ON
2. ANALYZE
3.
(SHOCK)
Manual button
Speed dial
Therapy cable connector
Back to contents
6 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Device maintenance
Most hospitals have specic protocols for maintaining their debrillators. Stryker
provides a variety of tools designed to help manage inspection and maintenance
procedures. Training for staff would depend on a hospital’s particular approach.
BLS-trained responders should be familiar with several of the device maintenance
procedures. How much detail you choose to go into will depend on your hospital’s
protocols.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
The case list contains the following columns:
Task
Check debrillator
for Daily Auto
Test results, if
congured on.
User action, debrillator labels, text/voice
prompts & information
• Ensure the debrillator is plugged in.
• Ensure the therapy cable is plugged into the
QUIK-COMBO test plug.
Or
• Ensure the standard paddles are clean, dry and
properly seated in the paddle wells and connected
to the debrillator.
If the debrillator detects a problem during the self-
test it will remain “on” if connected to AC power and
the SERVICE LED will illuminate and the printed
report will indicate SELF TEST FAILED.
If the debrillator detects a problem while on battery
power, the SERVICE LED will illuminate the next time
it is turned on.
Debrillator should be checked daily following the
auto test to conrm the test passed. If test failed or
incomplete perform the manual user test.
Task
Inspect the physical
condition of the
debrillator.
User action, debrillator labels, text/voice
prompts & information
Inspect Debrillator for damage and
foreign substances.
Task
Inspect power
source.
User action, debrillator labels, text/voice
prompts & information
Conrm that the AC Mains LED light is on
the LIFEPAK 20e debrillator/monitor and
CodeManagement Module (if applicable).
Task
Check therapy and
ECG electrodes.
User action, debrillator labels, text/voice
prompts & information
Check QUIK-COMBO and EGG electrodes for “use by”
date and that a spare set is available.
Task
Examine accessory
cables.
User action, debrillator labels, text/voice
prompts & information
Inspect all cables including power cord for cracks,
broken or bent parts and pins, and, if applicable,
paddle surfaces for pitting.
Task
Disconnect
debrillator from
AC power and wait
2 seconds.
Press ON.
Look for SELF-TEST
message and
illumination of LEDs.
User action, debrillator labels, text/voice
prompts and information
Debrillator turns on.
• If debrillator doesn’t turn on, contact qualied
service personnel.
• There should not be a LOW BATTERY CONNECT
TO AC POWER message visible. If visible, it may
mean the battery has reached its end-of-life
and needs replacing.
Back to contents
Instructor guide | 7
Task
Conrm that the
therapy cable
is connected to
debrillator and
perform cable
checks.
User action, debrillator labels, text/voice
prompts & information
For QUIK-COMBO cable:
1. Conrm that test plug is connected.
2. Press ANALYZE button. After ANALYZING NOW
message, look for REMOVE TEST PLUG message.
If CONNECT CABLE message appears, contact
qualied service personnel.
For Standard Paddles:
1. Conrm that paddles are properly seated in wells.
2. Select 10J and press CHARGE button on paddles.
3. When fully charged press (SHOCK) buttons on
paddles and look for ENERGY DELIVERED message.
If CONNECT CABLE message appears, contact
qualied service personnel.
Instructor activity
Disconnect
debrillator
from electricity.
Task
Reconnect the
debrillator to
AC power and
turn device off.
User action, debrillator labels, text/voice
prompts & information
Conrm AC MAINS LED is lit.
Task
Perform Manual
User Test.
Press ON.
Note: Ignore all
REMOVE TEST
PLUG prompts and
keep the test plug
connected for testing.
For QUIK-COMBO
pads:
• Conrm the QUIK-
COMBO therapy
cable is connected
to the QUIK-
COMBO test plug.
• Press OPTIONS.
• Select USER TEST.
• Select YES to
initiate user test.
For Hard Paddles:
• Conrm hard
paddles cable is
connected and
paddles are seated
rmly in the
paddle wells.
• Repeat steps
above under
QUIK-COMBO pads.
User action, debrillator labels, text/voice
prompts & information
The manual user test should be performed if hospital
protocol requires more frequent testing than the
recommended daily auto test, or the daily auto test
failed or did not complete, or if REDI-PAK™ electrodes
are connected to the therapy cable.
Note: If the debrillator is in AED mode, switch
to manual mode by opening the door or press the
ENERGY SELECT button.
Device will turn itself off after user test completed
and print results.
If the user test did not complete or self-tests failed,
contact a qualied service personnel.
Instructor activity
Conrm Test Plug
is connected to
QUIK-COMBO
cable or that
standard paddles
are seated rmly
in the paddle wells
Discuss
Cleaning
User action, debrillator labels, text/voice
prompts & information
Clean the LIFEPAK 20e debrillator/monitor, cables
and accessories with a damp sponge or cloth. Do not
use bleach. Use only the agents listed below:
• Quarternary ammonium compounds
• Isopropyl alcohol
• Peracetic (peroxide) acid solutions
Back to contents
8 | Instructor guide for the LIFEPAK 20e debrillator/monitor
AED operation
The AED mode on the LIFEPAK 20e debrillator/monitor is easy to use because it
automatically analyzes the patient’s heart rhythm and advises you which steps to take.
In AED mode the device automatically selects the appropriate energy dosing.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions.
Task
Verify the patient is
in cardiopulmonary
arrest: unconscious/
unresponsive, not
breathing normally,
and showing no signs
of circulation.
Press ON.
User action, debrillator labels, text/voice
prompts & information
Note the CONNECT ELECTRODES message and
voice prompt occurs until the patient is connected
to the device:
Task
Prepare the patient
for therapy electrode
placement.
Connect therapy
electrodes to the
therapy cable,
and conrm cable
connection to the
debrillator.
User action, debrillator labels, text/voice
prompts & information
• Bare patient’s chest.
• Remove excessive chest hair.
• Clean and dry skin.
• Abrade the skin briey using a dry towel or gauze
for better electrode adhesion to the skin.
• Do not use alcohol, tincture of benzoin, or
antiperspirant to prepare the skin.
Instructor activity
Connect therapy
cable to the rhythm
simulator and set
rhythm to VF
Task
Apply therapy
electrodes to
patient’s chest in
anterior-lateral
position.
Instructor activity
Conrm correct
placement
Task
Press ANALYZE
button to initiate
analysis. Stop CPR.
User action, debrillator labels, text/voice
prompts & information
You will see and hear the PUSH ANALYZE message.
• Stop all motion including CPR.
• Do not move the LIFEPAK 20e debrillator/monitor
while analyzing.
• Clear everyone away from patient.
Back to contents
Instructor guide | 9
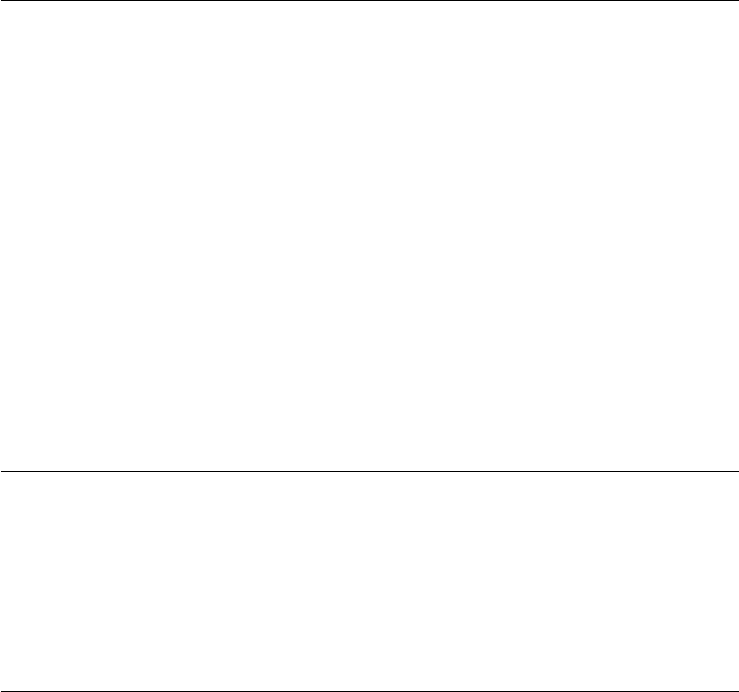
Task
Conrm everyone
is clear.
Press (Shock)
button to discharge
AED.
User action, debrillator labels, text/voice
prompts & information
You will see and hear ANALYZING NOW STAND
CLEAR, The AED analyzes the patient’s ECG and
advises either SHOCK ADVISED or NO SHOCK
ADVISED. If the AED detects a shockable rhythm, you
will see and hear SHOCK ADVISED.
1. State “All Clear” and observe that all personnel are
clear of the patient and immediate area.
2. Press (SHOCK) button to discharge AED.
When the is pressed, you will see Energy Delivered
message indicating energy transfer was completed.
Note: When energy transfer is complete, the shock
counter increases by 1. This will continue to increase
incrementally with every energy transfer.
Task
START CPR.
User action, debrillator labels, text/voice
prompts & information
START CPR screen message will appear.
• A CPR timer will countdown 2 minutes or CPR
time duration. A metronome automatically
provides 30:2 audible compression “tocks” and
ventilation prompts.
Instructor activity
Place rhythm
simulator in
non-shockable
rhythm
Task
The CPR metronome.
The CPR metronome provides audible “tocks” that
guide the user to deliver CPR with proper timing.
In AED Mode, the default C:V ratio is Adult – no
airway because most patients in cardiac arrest are
adults who have an initially unsecured airway. The
CPR metronome can not be turned off in AED Mode.
Task
Stop CPR and
push ANALYZE.
User action, debrillator labels, text/voice
prompts & information
When the CPR countdown time ends, you will see and
hear PUSH ANALYZE.
This message stays on the screen and the voice prompt
will repeat every 20 seconds until the ANALYZE
button is pressed.
Task
Conrm everyone
is clear.
User action, debrillator labels, text/voice
prompts & information
If the AED detects a nonshockable rhythm, you will
see and hear NO SHOCK ADVISED.
Task
START CPR.
User action, debrillator labels, text/voice
prompts & information
Start CPR per voice prompt and screen message.
• A CPR timer will countdown 2 minutes.
• Continue to follow screen messages and voice
prompts until the
Back to contents
10 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Discuss
Troubleshooting
messages.
User action, debrillator labels, text/voice
prompts & information
CONNECT ELECTRODES message and voice
prompt occur
• If therapy electrodes are not connected to the
therapy cable.
Or
• If therapy electrodes are not placed on the
patient’s chest.
CONNECT CABLE message occurs
• If the therapy cable is not connected to
the debrillator.
REMOVE TEST PLUG message and voice
prompt occurs
• If the test plug is connected to the therapy cable
when analysis is initiated. Remove test plug and
connect therapy electrodes to the therapy cable.
MOTION DETECTED, STOP MOTION message occurs
• If motion is detected during the ECG analysis,
you will see and hear MOTION DETECTED, STOP
MOTION, followed by a warning tone. Analysis
is inhibited
up to 10 seconds. After 10 seconds, even if motion
is still present, the analysis proceeds to completion.
Task
Switching from AED
to Manual Mode.
Switching from
Manual Mode
to AED mode.
User action, debrillator labels, text/voice
prompts & information
• Enter manual mode by pressing the MANUAL
button located in the lower left corner of the
door and opening door.
Or
• If there is no door, or the door is open, press
ENERGY SELECT button once to switch to
manual mode.
• Pressing ANALYZE while the device is in
manual mode will return device to AED mode.
Instructor activity
Have students
switch device
between AED and
manual mode and
back to AED mode
Back to contents
Instructor guide | 11
Manual training course
The manual mode training course is intended for the ALS-trained code team and reviews
the manual operation and functions of the LIFEPAK 20e debrillator/monitor. The
LIFEPAK 20e debrillator/monitor automatically converts to a manual debrillator
simply by opening a door and transitions easily to full therapy and monitoring capabilities.
This training course reviews all of the advanced cardiovascular life support tools available
in the LIFEPAK 20e debrillator/monitor.
Learning objectives
The overall objective of the in-service is to provide an overview of the basic steps of
operation of the identied controls, indicators, and connectors of the LIFEPAK 20e
debrillator/monitor. Upon completion of this course, participants will be able to:
• Verbalize the importance of early debrillation.
• Locate and identify the debrillator’s front panel controls, indicators and connectors.
• Demonstrate QUIK-COMBO electrode application.
• Demonstrate steps for manual debrillation.
• State the procedure for synchronized cardioversion.
• List the operational steps for noninvasive pacing.
• Demonstrate ECG, pulse oximetry, and EtCO
2
monitoring (if applicable).
• Describe the print process, transmitting, and recalling the code summary.
• Explain the power sources.
• Demonstrate routine daily testing.
Equipment and materials
The following is a list of accessories and support material recommended for ACLS training
on the LIFEPAK 20e debrillator/monitor. It is essential that all equipment be inspected
and tested to ensure proper function prior to training.
Equipment
• LIFEPAK 20e debrillator/monitor with Code Management Module (if applicable).
Accessories
• QUIK-COMBO therapy cable
• Test plug
• EDGE System™ electrodes with QUIK-COMBO connector
(or clip-on training electrodes)
• 3-lead or 12-lead patient simulator
• 3-wire or 5-wire ECG cable
• LIFEPAK 20e debrillator/monitor standard adult detachable
hard paddles (if applicable)
• SpO
2
sensors (if applicable)
• EtCO
2
cannula and T-piece connector
• AC power cord
• 50 mm ECG printer paper
Back to contents
12 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Support materials
• Quick reference cards
• Student study guide
• Operating instructions
• Performance evaluations
LIFEPAK 20e debrillator/monitor
Manual User Training Class
The following lists the content that should be covered during a typical
Manual User Training Class.
• Early debrillation
• Biphasic energy
• Controls and features
• Manual debrillation
• Synchronized cardioversion procedure
• Noninvasive pacing
• ECG monitoring
• Pulse oximetry (if applicable)
• EtCO
2
monitoring (if applicable)
• Data management
• Device maintenance
• Other functions
Early defibrillation
A New England Journal of Medicine study of 6,789 cardiac arrest patients reported 70%
received debrillation within 2 minutes. The survival rate declined for 30% of the patients
who received debrillation more than two minutes after their cardiac arrest.
1
The American Heart Association (AHA) Guidelines for cardiopulmonary resuscitation
recommended debrillation within 2 minutes of collapse in the hospital setting. The AHA
suggests hospitals deploy AEDs throughout the hospital to achieve the target time and
train staff to use the AEDs.
AEDs can help your hospital staff improve their ability to deliver the rst shock within
the recommended 2 minute guidelines. The LIFEPAK 20e debrillator/monitor can be
used in AED mode to debrillate without having to learn ECG interpretation. The AED
is simple to use because it is designed to automatically analyze the patient’s heart rhythm
and advise you which steps to take. In AED mode the device automatically selects the
appropriate energy dosing.
Back to contents

Instructor guide | 13
Biphasic energy
Health care providers may be confused about the right energy dose for biphasic
waveforms because different debrillator manufacturers recommend different energy
dosing protocols. It is important to clarify the correct recommended energy dose for
biphasic waveforms in order to avoid possible confusion that may result in a delay of
therapy. ADAPTIV biphasic technology provides the option to escalate to 360J for best
results. Studies show that rebrillation is common among ventricular brillation (VF)
CA patients and that debrillation of recurring episodes of VF is increasingly difcult.
2,3,4
LIFEPAK devices give you the option to escalate your energy dosing up to 360J for
difcult to debrillate patients.
Fortunately, all AEDs are programmed to follow a predened energy dosing protocol.
In other words, the healthcare provider doesn’t have to worry about energy dosing.
The AED performs this automatically.
A biphasic waveform sends current one way at the start of the shock and then reverses
it so the current ows in the opposite direction. A biphasic shock is a gentler but more
effective shock. Stryker recommends a dosing protocol of 200-300-360 joules and is
the factory default setting in all LIFEPAK debrillators. Stryker believes this energy
protocol can help minimize unnecessary CPR interruptions that result from ineffective
debrillation shocks.
Controls and features
In this section, the goal is to point out the different buttons and physical features pertinent
to an ALS user. Each of these features will be reviewed in greater detail in latter sections
of this guide. For complete information, review the Operating Instructions for the device.
Area 7
Area 1
Area 2
Area 3
Area 5
Area 4
Area 6
Back to contents
14 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Buttons
• ON
• ENERGY SELECT
• CHARGE
•
(SHOCK)
• SYNC
• ANALYZE
LED Light for AED Mode
Area 1
ON
Switches power on or off.
ENERGY SELECT
Selects energy levels in manual mode.
CHARGE
Charges the debrillator in
manual mode.
SHOCK
Discharges debrillator energy
to the patient.
SYNC
Activates synchronized mode.
ANALYZE
Activates Shock Advisory System (SAS).
AED MODE
LED illuminates when AED mode is active.
Back to contents
16 | Instructor guide for the LIFEPAK 20e debrillator/monitor
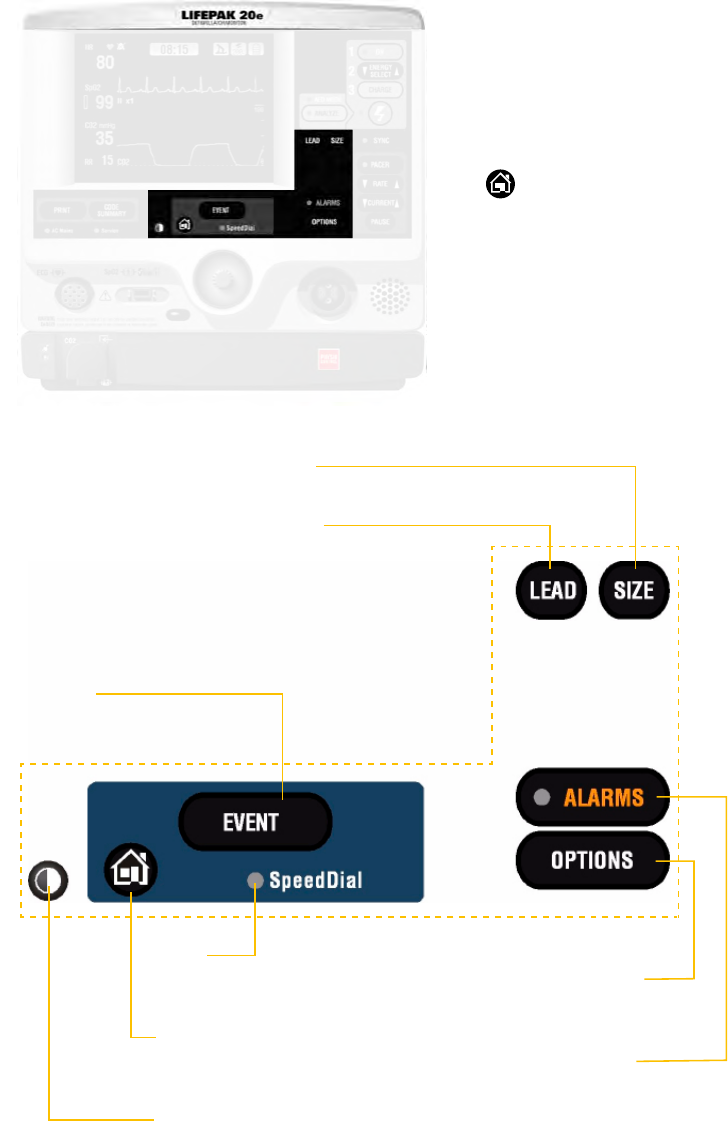
Area 3
Buttons
• EVENT
• LEAD
• SIZE
• ALARMS
• OPTIONS
•
(Home screen)
LED Light for Speed Dial
EVENT
Activates user-dened events.
LED
Illuminates when the
Speed Dial is active.
Home screen
Returns immediately to
home screen.
Contrast
Adjusts screen contrast.
OPTIONS
Accesses optional
functions.
ALARMS
Activates and
silences alarms.
SIZE
Changes ECG size.
LEAD
Changes ECG lead
Back to contents
Instructor guide | 17
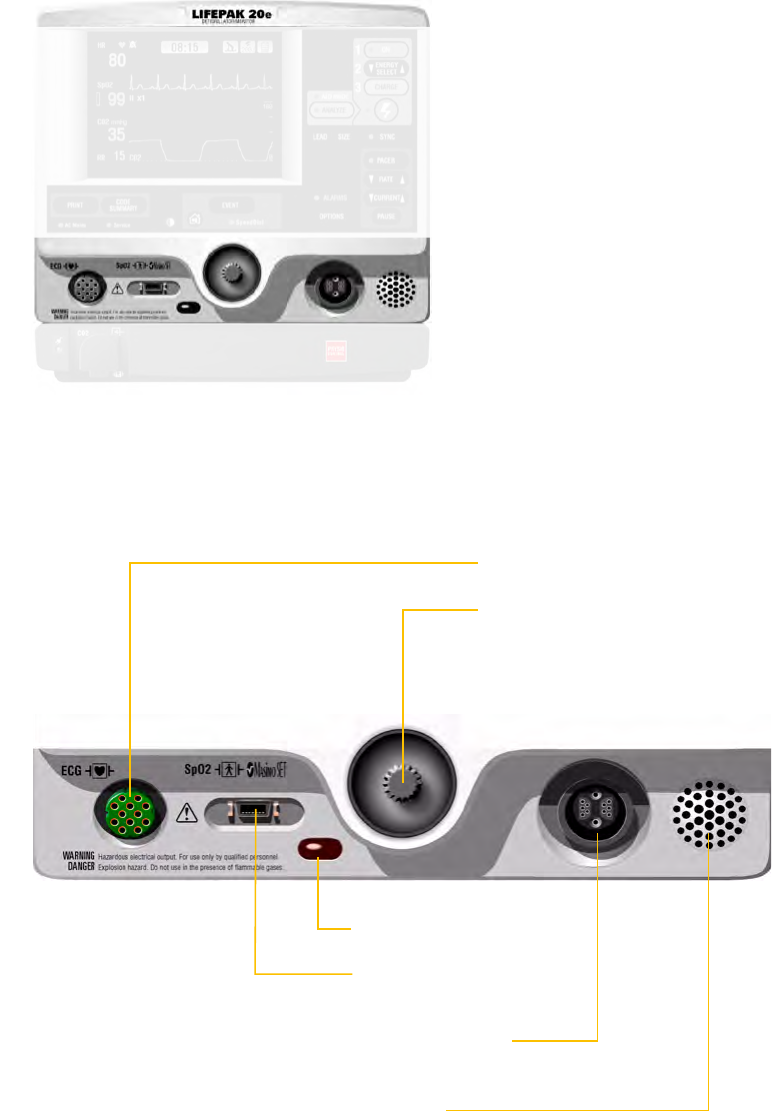
Area 4
• ECG cable connector
• SpO
2
cable connector
(if applicable)
• Therapy cable connector
• Speed dial
• IrDA port
• Speaker
Ecg cable receptacle
Speed dial
Scrolls through and selects
menu items. LED illuminates
when Speed Dial is active.
IrDA port
SpO
2
cable
receptacle
Therapy cable
receptacle
Speaker
Back to contents

18 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Area 5
• PRINT
• CODE SUMMARY
LED Light for AC Mains and Service
PRINT
Starts or stops the printer.
CODE SUMMARY
Prints a CODE SUMMARY
critical event record.
Service
Indicates that service is required.
AC Mains
LED illuminates when AC power
(line power) is connected and
providing power.
Back to contents
20 | Instructor guide for the LIFEPAK 20e debrillator/monitor
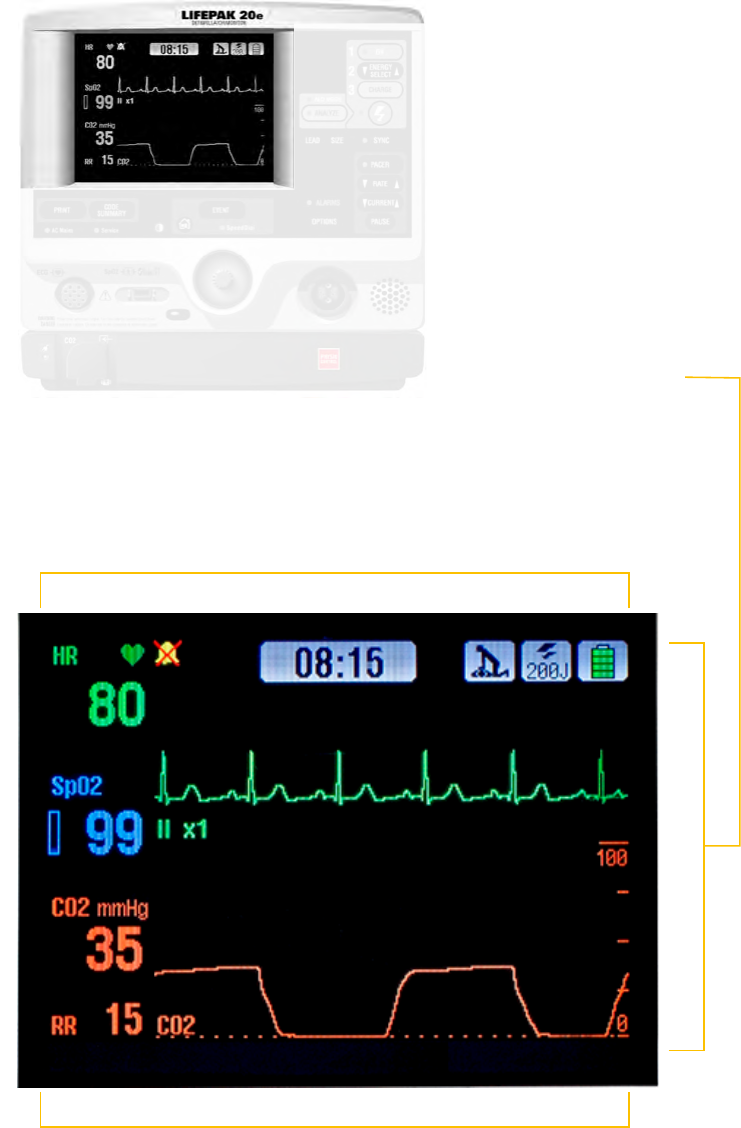
Area 7
• Monitoring area
• Waveform channel area
• Status message area
Channel 1
Channel 2
Monitoring area
Displays heart rate, time, SpO
2
, battery status indicator,
indicators for VF/VT alarm and selected energy.
Status message area
Displays status and alarm messages.
Waveform
channel area
Displays up to
two waveform
channels.
Back to contents
Instructor guide | 21
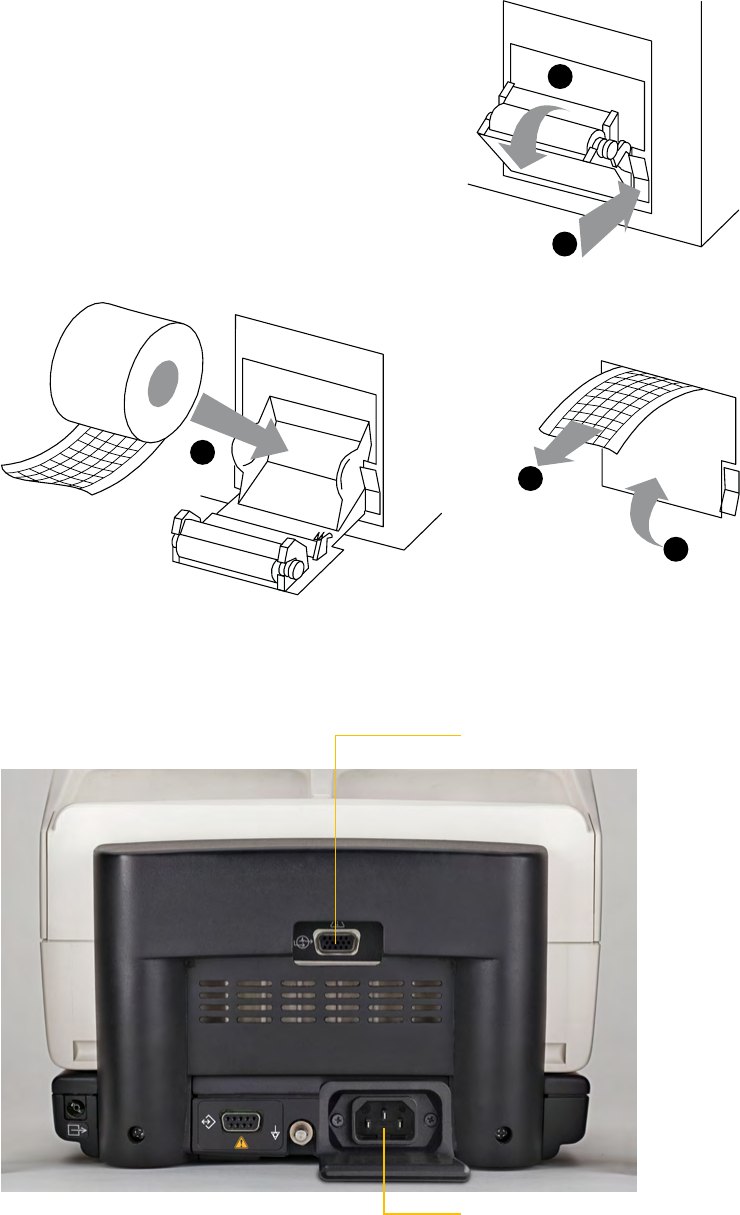
Additional areas not shown
Door with manual access button (if applicable)
Left side
• Printer
To load the paper:
1. Press the black button to open the printer door.
2. Remove the empty paper roll.
3. Insert the new paper roll, grid facing upward.
4. Pull out a short length of paper.
5. Push the printer door in to close.
Back view with the CodeManagement Module
• AC power cord connection
• ECG/SYNC connector
1
2
3
4
5
ECG/SYNC connector
AC power cord connection
Back to contents
22 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Device maintenance
Most hospitals have specic protocols for maintaining their debrillators. Stryker
provides a variety of tools designed to help manage inspection and maintenance
procedures. Training for staff would depend on a hospital’s particular approach.
BLS-trained responders should be familiar with several of the device maintenance
procedures. How much detail you choose to go into will depend on your hospital’s protocols.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
Check debrillator
for Daily Auto Test
results, if
congured on.
User action, debrillator labels, text/voice
prompts & information
• Ensure the debrillator is plugged in.
• Ensure the therapy cable is plugged into the
QUIK-COMBO test plug.
Or
• Ensure the standard paddles are clean, dry and
properly seated in the paddle wells and connected
to the debrillator.
If the debrillator detects a problem during the self-
test it will remain “on” if connected to AC power and
the SERVICE LED will illuminate and the printed
report will indicate SELF TEST FAILED.
If the debrillator detects a problem while on battery
power, the SERVICE LED will illuminate the next time
it is turned on.
Debrillator should be checked daily following the
auto test to conrm the test passed. If test failed or
incomplete perform the manual user test.
Task
Inspect the physical
condition of the
debrillator.
User action, debrillator labels, text/voice
prompts & information
Inspect Debrillator for damage and
foreign substances.
Task
Inspect Power
Source.
User action, debrillator labels, text/voice
prompts & information
Conrm that the AC Mains LED light is on
the LIFEPAK 20e debrillator/monitor and
CodeManagement Module (if applicable).
Task
Check therapy and
ECG electrodes.
User action, debrillator labels, text/voice
prompts & information
Check QUIK-COMBO and EGG electrodes for “use by”
date and that a spare set is available.
Task
Examine accessory
cables.
User action, debrillator labels, text/voice
prompts & information
Inspect all cables including power cord for cracks,
broken or bent parts and pins, and, if applicable,
paddle surfaces for pitting.
Task
Disconnect
debrillator from AC
power and wait 2
seconds.
Press ON.
Look for SELF-
TEST message and
illumination of LEDs.
User action, debrillator labels, text/voice
prompts & information
Debrillator turns on.
• If debrillator doesn’t turn on, contact qualied
service personnel.
• There should not be a LOW BATTERY CONNECT
TO AC POWER message visible. If visible, it may
mean the battery has reached its end-of-life
nd needs replacing.
Back to contents
Instructor guide | 23
Task
Conrm that the
therapy cable
is connected to
debrillator and
perform cable
checks.
User action, debrillator labels, text/voice
prompts & information
For QUIK-COMBO cable:
1. Conrm that test plug is connected.
2. Press ANALYZE button. After ANALYZING NOW
message, look for REMOVE TEST PLUG message.
If CONNECT CABLE message appears, contact
qualied service personnel.
For Standard Paddles:
1. Conrm that paddles are properly seated in wells.
2. Select 10J and press CHARGE button on paddles.
3. When fully charged press (SHOCK) buttons on
paddles and look for ENERGY DELIVERED message.
If CONNECT CABLE message appears, contact
qualied service personnel.
Instructor activity
Disconnect
debrillator
from electricity.
Task
Reconnect the
debrillator to AC
power and turn
device off.
User action, debrillator labels, text/voice
prompts & information
Conrm that the AC Mains LED light is on
the LIFEPAK 20e debrillator/monitor and
CodeManagement Module (if applicable).
Task
Perform Manual
User Test.
Press ON.
Note: Ignore all
REMOVE TEST
PLUG prompts and
keep the test plug
connected for testing.
For QUIK-COMBO
pads:
• Conrm the
QUIK-COMBO
therapy cable is
connected to the
QUIK-COMBO
test plug.
• Press OPTION.
• Select USER TEST.
• Select YES to
initiate user test.
For Hard Paddles:
• Conrm hard
paddles cable is
connected and
paddles are seated
rmly in the paddle
wells.
• Repeat steps
above under
QUIK-COMBO pads.
User action, debrillator labels, text/voice
prompts & information
The manual user test should be performed if hospital
protocol requires more frequent testing than the
recommended daily auto test, or the daily auto test
failed or did not complete, or if REDI-PAK™ electrodes
are connected to the therapy cable.
Note: If the debrillator is in AED mode, switch
to manual mode by opening the door or press the
ENERGY SELECT button.
Device will turn itself off after user test completed
and print results.
If the user test did not complete or self-tests failed,
contact a \qualied service personnel.
Note: For additional Function Checks consult the
Operating Instructions
Instructor activity
Conrm Test Plug
is connected to
QUIK-COMBO cable
or that standard
paddles are seated
rmly in the
paddle wells
Discuss
Cleaning
User action, debrillator labels, text/voice
prompts & information
Clean the 20e debrillator/monitor, cables and
accessories with a damp sponge or cloth. Do not use
bleach. Use only the agents listed below:
• Quarternary ammonium compounds
• Isopropyl alcohol
• Peracetic (peroxide) acid solutions
Back to contents
24 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Manual defibrillation
A direct current debrillator applies a brief, intense pulse of electricity to the heart muscle.
The LIFEPAK 20e debrillator/monitor delivers this energy through disposable electrodes,
standard paddles or internal paddles applied to the patient’s chest. Debrillation is only
one aspect of the medical care required to resuscitate a patient with a shockable ECG
rhythm. Depending on the situation, other supportive measures may include:
• High performance CPR
• Waveform capnography and ventilation support
• Drug therapy
Successful resuscitation is related to the length of time between the onset of a heart
rhythm that does not circulate blood (ventricular brillation, pulseless ventricular
tachycardia) and debrillation. Having an AED on site and knowing CPR are so important
that the American Heart Association includes both in their chain of survival. AHA
recommends the chain of survival as follows:
1. Immediate recognition of cardiac arrest and activation of the
emergency response system
2. Early cardiopulmonary resuscitation (CPR) with an emphasis
on high-quality chest compressions
3. Rapid debrillation
4. Effective advanced life support
5. Integrated post-cardiac arrest care
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
Verify the patient is
in cardiopulmonary
arrest: unconscious/
unresponsive, not
breathing normally,
and showing no
signs of circulation
after arrest.
Press ON.
Task
Connect therapy
electrodes to the
therapy cable,
and conrm cable
connection to the
debrillator.
Instructor activity
Connect therapy
cable to the
simulator and set
rhythm to VF
Back to contents
Instructor guide | 25
Task
Prepare the patient
for therapy electrode
placement.
Apply therapy
electrodes to
patient’s chest in
anterior-lateral
position.
Note: If needed,
refer to anterior-
lateral placement,
section 4 of
the Operating
Instructions.
User action, debrillator labels, text/voice
prompts & information
• Remove all clothing from the patient’s chest.
• Remove excessive chest hair.
• Clean and dry the skin.
• Do not use alcohol, tincture of benzoin, or
antiperspirant to prepare the skin.
• Ensure pads are in sealed package and the
use by date has not passed.
• Avoid placement over the nipple, bony
prominences, dressings, implantable
debrillators, or the diaphragm if possible.
• Apply therapy electrodes to patient’s chest
in anterior-lateral position.
• If using standard paddles, apply conductive
gel to the electrodes and place paddles on the
patient’s chest.
Note: Impedance is measured whenever the
debrillator is charged. To ensure therapeutic
patient impedance levels, you should always
charge the debrillator when the standard paddle
or QUIK-COMBO electrodes are in contact with
the patient’s chest.
Instructor activity
Demonstrate anterior
lateral position with
therapy electrodes
Task
Press ENERGY
SELECT.
User action, debrillator labels, text/voice
prompts & information
Select joules per protocols.
Task
Press CHARGE.
Press SPEED DIAL
to disarm.
User action, debrillator labels, text/voice
prompts & information
While the debrillator is charging, a charging
bar appears and a ramping tone sounds,
ndicating the charging energy level.
When debrillator is fully charged, an
overlay appears.
Task
Make certain all
personnel, including
the operator, stand
clear of the patient,
bed, and any
equipment connected
to the patient.
Press the
(SHOCK) button to
discharge energy to
the patient.
User action, debrillator labels, text/voice
prompts & information
State “All Clear” and observe that all personal
are clear of the patient and immediate area.
Conrm ECG rhythms and available energy.
Discuss
To change energy
selection.
User action, debrillator labels, text/voice
prompts & information
If energy selection is changed after charging has
started, the energy is removed. Press CHARGE
to restart charging.
Back to contents
26 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Synchronized cardioversion procedure
The LIFEPAK 20e debrillator/monitor can be congured to remain in synchronous mode
or to return to asynchronous mode after discharge. It is important that you know how
your debrillator is congured.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
Press ON.
Task
Attach patient ECG
cables and ECG
electrodes on the
patient.
Select Lead II or the
lead with greatest
QRS complex
amplitude (positive
or negative).
Observe the ECG
rhythm.
Press SYNC.
Observe the ECG
rhythm.
Prepare the patient’s
skin for therapy
electrode application.
Connect the therapy
electrodes to the
therapy cable,
conrm cable
connect to the
device.
Apply therapy
electrodes to the
patient in the
anterior-lateral
position. If using
standard paddles,
apply conductive gel
to the paddles and
place paddles on the
patient’s chest.
User action, debrillator labels, text/voice
prompts & information
• Bare patient’s chest.
• Ensure chest is clean and dry.
• Remove excessive chest hair.
• Prepare electrode site with brisk rub.
• Ensure electrodes are in sealed package
and the use by date has not passed.
• Avoid placement over the nipple, bony
prominences, dressings, implantable
debrillators, or the diaphragm if possible.
Note: To monitor the ECG through therapy electrodes,
place the electrodes in the anterior-lateral position
and select paddles lead.
Conrm the Sync LED blinks with each detected
QRS complex. Note: Press SYNC again to deactivate
synchronous mode.
Conrm that a triangle sense marker appears near the
middle of each QRS complex. If the sense markers do
not appear or are displayed in the wrong locations (for
example, on the T-wave), select another lead.
Instructor activity
Connect QUIK-
COMBO Therapy
Cable to the
simulator and set
rhythm to VT
Task
Press ENERGY
SELECT.
User action, debrillator labels, text/voice
prompts & information
Select joules per protocols.
Task
Press CHARGE.
User action, debrillator labels, text/voice
prompts & information
If the REMOVE TEST PLUG message appears,
disconnect test plug and connect therapy electrodes
to QUIK-COMBO therapy cable and press CHARGE.
Back to contents
Instructor guide | 27
Task
Make certain all
personnel, including
operator, stand
clear of the patient,
bed, and any
equipment connect
to the patient.
Conrm rhythm and
available energy.
Task
Press and hold
(SHOCK)
button(s) until
you see ENERGY
DELIVERED on
screen.
User action, debrillator labels, text/voice
prompts & information
If (SHOCK) buttons are not pressed within
60 seconds, stored energy is internally removed.
Note: If the energy selection is changed after charging
has started, the energy is removed internally. Press
CHARGE to restart charging
Back to contents
28 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Noninvasive pacing
The noninvasive pacemaker can be used for either demand (synchronous) or nondemand
(asynchronous) pacing modes.
The demand mode is used for most patients. In the demand mode, the LIFEPAK 20e
debrillator/monitor/pacemaker inhibits pacing when it senses the patient’s own beats, if the
ECG amplitude is too low to detect the patient’s beats, or if an ECG lead becomes detached so
that the ECG rhythm is not present, the pacemaker generates pacing pulses asynchronously.
ECG monitoring during pacing must be performed with the ECG electrodes and patient
ECG cable. Pacing therapy electrodes cannot be used to monitor ECG rhythm and deliver
pacing current at the same time. Be sure to place the therapy electrodes in the proper
locations as described in the pacing procedure. Improper electrode placement may make
a difference in the capture threshold.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
Press ON.
Instructor activity
Connect QUIK-
COMBO Therapy
Cable to the
simulator and
set rhythm to
bradycardia
Task
Connect the patient
ECG cable, apply
ECG electrodes to
the ECG cable and
patient, and select
Lead I, II, or III.
Identify the QUIK-
COMBO electrode
sites on the patient.
Prepare patient’s
skin for electrode
application.
Apply QUIK-COMBO
electrodes to the
patient.
Connect the therapy
electrodes to the
therapy cable.
User action, debrillator labels, text/voice
prompts & information
To receive the best monitoring signal, ensure there is
adequate space between the ECG electrodes and the
QUIK-COMBO electrodes.
For pacing, use either the anterior-lateral or anterior-
posterior position.
Task
Press the PACER
button.
Observe the ECG
rhythm.
User action, debrillator labels, text/voice
prompts & information
Conrm the PACER LED illuminates, indicating that
the power is on.
Note: If the REMOVE TEST PLUG message appears,
disconnect the test plug and connect therapy
electrodes to QUIK-COMBO therapy cable.
Conrm that a triangle sense marker appears near the
middle of each QRS complex. If the sense markers do
not appear or are displayed in the wrong location (i.e.:
T wave) select another lead.
Back to contents
Instructor guide | 29
Task
Press the RATE
button.
User action, debrillator labels, text/voice
prompts & information
• Turn SPEED DIAL (changes rate in increments
of 5 ppm) or press RATE button (changes rate in
increments of 10 ppm) to desired pacing rate.
• Pacing rate range from 40 to 170 ppm.
• Set rate to 80 ppm
Task
Press the CURRENT
button.
User action, debrillator labels, text/voice
prompts & information
Turn SPEED DIAL (changes current in increments
of 5mA) or press CURRENT button (changes rate
in increments of 10mA) to increase current until
electrical capture occurs.
• For each delivered pacing stimulus, the PACER
indicator ashes off and a positive pace marker
displays on the ECG waveform.
• Pacing current range from 0 to 200mA.
• Many patients achieve capture at 50 to 100mA,
although individual thresholds vary. The simulator
achieves electrical capture at 65mA.
Task
Assess for
mechanical capture.
User action, debrillator labels, text/voice
prompts & information
Both electrical and mechanical capture must occur in
order for noninvasive pacing to benet the patient.
• Palpate patients pulse and obtain blood pressure to
assess for mechanical capture.
• Compare the SpO
2
pulse rate with the set pacing
rate to assess for mechanical capture.
• Consider use of sedation/analgesia if necessary for
patient discomfort.
User action, debrillator labels, text/voice
prompts & information
Note: To interrupt pacing and view the patient’s
intrinsic rhythm, press and hold the PAUSE button.
This causes the pacer to pace at 25% of the set rate.
Release the PAUSE button to resume pacing at the set
rate. An ECG strip prints automatically for as long as
the button is held.
Task
To stop pacing.
User action, debrillator labels, text/voice
prompts & information
To stop pacing reduce current to zero or press PACER.
To debrillate and stop noninvasive pacing, press the
ENERGY SELECT button or charge the debrillator.
Pacing automatically stops.
Proceed with debrillation.
Instructor activity
Set simulator to
VF and demonstrate
debrillation
while pacing.
Back to contents
30 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Discuss
Troubleshooting
• User observation.
• ECG leads off
during pacing.
User action, debrillator labels, text/voice
prompts & information
If the monitor detects ECG leads off during pacing,
pacing continues at a xed rate (nondemand pacing)
until the ECG lead is reattached. During xed-rate
pacing, the pacemaker delivers pulses at the set pace
rate regardless of any intrinsic beats that the patient
may have. The monitor continues to display the
pacing rate (ppm) and the current (mA). To reestablish
demand pacing, reattach the ECG lead.
While pacing, visually monitor the patient at all times,
do not rely on the ECG LEADS OFF warning to detect
changes in pacing function. Routinely assess the ECG
for proper sensing, pace pulse delivery, electrical and
mechanical capture.
Task
QUIK-COMBO
electrodes off
during pacing.
User action, debrillator labels, text/voice
prompts & information
If the therapy electrodes detach during pacing, the
CONNECT ELECTRODES and PACING STOPPED
messages appear and an alarm sounds. The pacing
rate is maintained and the current resets to 0mA.
Reattaching the electrodes silences the alarm and
removes the CONNECT ELECTRODES message.
The current remains at 0mA until the current is
increased manually.
Instructor activity
Disconnect LL lead
from simulator
Back to contents
Instructor guide | 31
ECG monitoring
There are two methods for selecting or changing the ECG lead. Both methods are available
on your LIFEPAK 20e debrillator/monitor. The leads available depend on the ECG cable
(3-wire or 5-wire) connected to the debrillator.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
Press ON.
Task
Attach the ECG cable
to the monitor
User action, debrillator labels, text/voice
prompts & information
Instructor activity
Connect ECG
cable leads to
the simulator and
choose a rhythm
Task
Identify the
appropriate electrode
sites on the patient
User action, debrillator labels, text/voice
prompts & information
Prepare the patient skin for electrode application:
• Remove excessive hair at electrode site. Avoid
placing electrodes over tendons and major
muscle masses.
• For oily skin, clean skin with an alcohol pad.
• Dry the site with a brisk rub.
Task
Apply ECG electrodes
User action, debrillator labels, text/voice
prompts & information
• Conrm package is sealed and use by date has not
passed.
• Attach an electrode to each lead wire.
• Grasp electrode tab and peel electrode from carrier.
• Inspect electrode gel for moisture content and to
conrm gel is intact.
• Apply the electrode at to skin. Smooth
tape outwardly. Avoid pressing the center
of the electrode.
• Secure the trunk cable clasp to the
patient’s clothing.
Task
Select the lead on the
monitor screen
User action, debrillator labels, text/voice
prompts & information
• Channel 1 Top channel displays the primary ECG
waveform and is always visible when ECG is
displayed.
• Lead options available are dependent on use of a 3
wire or 5 wire cable.
• Change lead by pressing the LEAD button and
select the desired lead with the SPEED DIAL. Or by
pressing the LEAD button.
• Adjust the ECG size by pressing the SIZE button
and select the size with the SPEED DIAL, or by
pressing the SIZE button.
Back to contents
32 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Task
Optional: Channel 2
waveform
User action, debrillator labels, text/voice
prompts & information
• This can display an additional waveform
or a continuation of the Channel 1 ECG.
• At the home screen, rotate the SPEED DIAL
to highlight Channel 2.
• Press the SPEED DIAL. An overlay appears with
the monitoring choice for the selected channel.
• Rotate and press the SPEED DIAL to select
monitoring choice.
Task
Adjusting the Systole
Tone Volume.
User action, debrillator labels, text/voice
prompts & information
Highlight and select heart rate (HR) in the monitoring
area of the screen.
• Rotate the SPEED DIAL to the desired volume.
• Press the (icon) HOME SCREEN to exit.
Discuss
• Press PRINT
to obtain an
ECG printout.
User action, debrillator labels, text/voice
prompts & information
Prints continuously until you press the PRINT button
again to stop printing.
Back to contents
Instructor guide | 33
Optional feature: Pulse oximetry
A pulse oximeter is a noninvasive tool that checks the saturation of oxygen in arterial
blood (SpO2) and is not to be used as an apnea monitor. It is used for monitoring
patients who are at risk of developing hypoxemia. Pulse oximetry can be used in
addition to patient assessment. If a trend toward patient deoxygenation is indicated,
blood samples should be analyzed using laboratory instruments to completely
understand the patient’s condition.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
Connect the SpO
2
cable to the monitor.
User action, debrillator labels, text/voice
prompts & information
Attach the sensor to the SpO
2
cable and the patient.
Task
Turn the debrillator
ON.
User action, debrillator labels, text/voice
prompts & information
When the debrillator is turned on, the oximeter
turns on and performs a self-test that requires up
to 10 seconds. A sleep mode is activated within
10 seconds of disconnecting the sensor. The oximeter
will return to normal mode after detecting a sensor
or a patient signal.
Task
Observe the pulse
bar for uctuation.
User action, debrillator labels, text/voice
prompts & information
Amplitude of the pulse bar indicates relative
signal strength.
Task
Display waveform.
User action, debrillator labels, text/voice
prompts & information
• Select waveform channel 2 using the SPEED DIAL.
• Select SpO
2
from the Waveform menu.
• The SpO
2
waveform automatically sizes
itself to provide optimum waveform viewing.
Task
Adjust SpO
2
volume.
User action, debrillator labels, text/voice
prompts & information
Highlight and select SpO
2
on the home screen with the
SPEED DIAL:
• Highlight and select SpO
2
VOLUME.
• Rotate the SPEED DIAL to the desired volume.
• Press the SPEED DIAL to set the volume.
Task
Adjust sensitivity.
User action, debrillator labels, text/voice
prompts & information
Highlight and select SpO
2
on the home screen with the
SPEED DIAL and then select SENSITIVITY.
• Normal sensitivity is the default.
• High sensitivity allows monitoring in low perfusion
states, but is more susceptible to artifact.
Task
Adjust averaging
time.
User action, debrillator labels, text/voice
prompts & information
• Highlight and select SpO
2
on the home screen with
the SPEED DIAL and select AVERAGING TIME.
• Turn the SPEED DIAL to select and set
averaging time.
Options:
1. 4 seconds (for patients with rapidly
changing values)
2. 8 seconds (recommended for most patients)
3. 12 and 16 seconds (when artifact is affecting
the performance of the pulse oximeter)
Back to contents
34 | Instructor guide for the LIFEPAK 20e debrillator/monitor
Optional feature: EtCO2
The end-tidal CO
2
(EtCO
2
) monitor is a capnometric device that uses non-dispersive
infrared spectroscopy to continuously measure the amount of CO
2
during each breath and
report the amount present at the end of exhalation (EtCO
2
). The sample is obtained by the
side stream method and can be used with intubated or nonintubated patients. Respiration
rate is also measured and displayed in breaths per minute.
EtCO
2
monitoring is used to detect trends in the level of expired CO
2
. It is used for
monitoring breathing efcacy and treatment effectiveness in acute cardiopulmonary care,
for example, to determine if adequate compressions are being performed during CPR or to
rapidly detect whether an endotrachael tube has been placed successfully.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Capnography monitoring is available with the CodeManagement Module.
Discuss
To monitor EtCO
2
:
Press ON.
User action, debrillator labels, text/voice
prompts & information
1. Select the appropriate EtCO
2
accessory for
the patient.
2. Open the CO
2
port door and insert the FilterLine
connector; turn connector clockwise until
hand tight.
3. Verify that the CO
2
area is displayed. The EtCO
2
monitor performs the autozero routine as part of
the initialization self-test.
4. Display CO
2
waveform in channel 2.
5. Connect the CO
2
FilterLine set to the patient.
6. Conrm that the EtCO
2
value and waveform are
displayed. The monitor automatically selects the
scale for the best visualization of the waveform.
Task
To display the
EtCO
2
waveform.
User action, debrillator labels, text/voice
prompts & information
1. Rotate the SPEED DIAL to outline display
channel 2.
2. Press the SPEED DIAL.
3. Select WAVEFORM.
4. Rotate the SPEED DIAL to select CO
2
.
5. Press the SPEED DIAL.
6. Press the HOME SCREEN button to clear
the menu.
Task
To change the
CO
2
scale:
User action, debrillator labels, text/voice
prompts & information
1. Rotate the SPEED DIAL to outline CO
2
area.
2. Press the SPEED DIAL.
3. Select SCALE.
4. Rotate the SPEED DIAL to select the desired scale.
• Autoscale (default)
• 0–20 mmHg (0–4 Vol% or kPa)
• 0–50 mmHg (0–7 Vol% or kPa)
• 0–100 mmHg (0–14 Vol% or kPa)
5. Press the SPEED DIAL to set the scale.
6. Press the HOME SCREEN button to clear
the menu.
Back to contents
Instructor guide | 35
Data management
When you turn on the LIFEPAK 20e debrillator/monitor, you create a new Patient Record
stamped with the current date and time. All events and associated waveforms are digitally
stored in the Patient Record as patient reports. When you turn the device off, the current
Patient Record data is saved in the patient archives.
The Patient Record can be printed for storage in the patient’s paper le. It can also be
uploaded and reviewed on a computer with CODE-STAT™ Data Review Software with
Advanced CPR Analytics. This feature allows the user to collect, manage, and analyze post-
event CPR performance and can help your hospital manage quality assurance and improve
responder performance.
Hospitals have different approaches to managing patient data. The training for your staff
will depend on your hospital’s particular approach.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
EVENT
User action, debrillator labels, text/voice
prompts & information
Pressing EVENT displays a menu showing drug
names or activities that may have been given or
done during the debrillator use. Use the Speed Dial
to scroll through and select the menu choices.
The selected event and time stamp appear in the
message area on the screen and are printed in the
CODE SUMMARY Event Log.
Task
CODE SUMMARY™
Critical Event Record
User action, debrillator labels, text/voice
prompts & information
A CODE SUMMARY report is automatically stored as
part of the patient record for each patient. The report
consists of:
• Preamble Contains patient demographic and
device information. The event identication
composed of the date and time the debrillator is
turned on, is automatically entered in the ID eld.
• Event/Vital Signs Log Contains events and vital
signs in chrono logical order. Events are device or
operator actions that are related to the use of the
debrillator. Vital signs (HR, SpO
2
saturation, and
EtCO
2
values) are entered into the log automatically
every 5 minutes.
• Waveform Events Therapy and other selected
events also capture waveform data. Refer to the
Operating Instructions for more detail.
Instructor activity
Press CODE
SUMMARY to print
a code summary for
the current patient.
Task
Managing Archived
Patient Records.
Press OPTIONS.
Select ARCHIVES.
User action, debrillator labels, text/voice
prompts & information
Data Storage: When the LIFEPAK 20e debrillator/
monitor is turned on, a new patient record is created.
The report is automatically stamped with the patient
ID and is saved in ARCHIVES when the debrillator is
turned off.
When Archives is entered, patient monitoring ends
and the current patient record is saved and closed.
• Send Data Allows wireless transmission of
patient data for selected patient (available with
CodeManagement Module)
• Print Allows printing of CODE SUMMARY for
selected patient.
• Edit Allows editing of selected elds in the patient
record such as name, ID, sex, etc.
• Delete Allows deletion of selected patient records.
Back to contents
Instructor guide | 37
Other functions
Setup options allow you to dene operating features for the LIFEPAK 20e debrillator/
monitor such as device identication numbers and default settings.
References to buttons are indicated in BOLD and display messages are indicated in
ITALICS. For complete information, review the Operating Instructions for the device.
Task
Setting alarms
User action, debrillator labels, text/voice
prompts & information
• Press ALARMS.
• Select QUICK SET to activate the alarms for
all active parameters (HR, SpO2, and EtCO
2
if applicable).
• Select LIMITS to set or change the alarm limits
to WIDE or NARROW.
• Limits are set based on the patient’s current HR
and SpO
2
saturation.
• Select SUSPEND to turn off the audible alarm
tone for up to 15 minutes.
• Select VF/VT ALARM to turn on continuous
monitoring for ventricular brillation and
ventricular tachycardia in manual mode.
• A symbol (magnifying glass) appears above the
primary ECG when the alarm is on.
Task
Managing alarms
User action, debrillator labels, text/voice
prompts & information
• The alarm bell symbol indicates when alarms are
ON or OFF. When Alarms are OFF a red X appears
over the bell.
• When alarms are on and an alarm limit is exceeded,
a tone sounds, the violated parameter ashes, and
an alarm message appears.
To manage an alarm:
• Press ALARMS. This silences the alarm tone for
2 minutes.
• Assess the cause of the alarm.
• Assess the appropriateness of the limits setting
(WIDE or NARROW).
• If the patient is unstable, consider suspending
the alarm tone for up to 15 minutes. Do not
reselect QUICK SET.
• Once the patient is stable reselect QUICK SET
if necessary.
Task
Options
User action, debrillator labels, text/voice
prompts & information
Pressing OPTIONS displays a menu showing the
following items. Use the Speed Dial to scroll through
and select the menu choices.
• PATIENT Allows entering of patient demographic
information into the patient record.
• PACING Selects demand or nondemand pacing
and internal pacer detection on or off.
• PRINT Allows printing of CODE SUMMARY
reports.
• ARCHIVES Accesses archived patient records.
• DATE/TIME Sets the date and time. For changes
to take effect, cycle power.
• ALARM VOLUME Adjusts volume for alarms,
tones, and voice prompts.
Back to contents

Instructor guide | 39
LIFEPAK
®
20e Debrillator/Monitor with and without
CodeManagement Module
®
BRIEF SUMMARY OF INDICATIONS AND IMPORTANT SAFETY INFORMATION
LIFEPAK 20e debrillator/monitor is an acute cardiac care response system intended for use by authorized
healthcare providers in hospital and clinic settings. It is to be used on one patient at a time. LIFEPAK 20e is intended
for use by personnel who have been trained in its operation. AED MODE. Indications for Use: To be used only on
patients in cardiopulmonary arrest. Patient must be unconscious, pulseless, and not breathing normally before using
debrillator to analyze patient’s ECG rhythm. In AED mode, LIFEPAK 20e is not intended for use on pediatric patients
less than 8 years old. Contraindications: None known. Operator Considerations: In AED mode, LIFEPAK 20e is
intended for use by personnel authorized by physician/medical director and have, at a minimum, the following: CPR
training, AED training equivalent to that recommended by AHA, and training in use of LIFEPAK 20e in AED mode.
DEFIBRILLATION THERAPY. Indications for Use: Debrillation is a recognized means of terminating certain
potentially fatal arrhythmias, such as VF and symptomatic VT. Delivery of this energy in synchronized mode is a
method for treating AF, atrial utter, paroxysmal supraventricular tachycardia, and, in relatively stable patients,
VT. Contraindications: Treatment of PEA such as idioventricular or ventricular escape rhythms, and in treatment
of asystole. Operator Considerations: LIFEPAK 20e delivers energy through disposable electrodes, standard
paddles applied to a patient’s chest, or internal paddles applied directly to the patient’s heart. Debrillation is only
one aspect of medical care required to resuscitate patient with shockable ECG rhythm. Other supportive measures
may include CPR, administration of supplemental oxygen and drug therapy. NONINVASIVE PACING. Indications
for Use: For symptomatic bradycardia in patients with pulse. Contraindications: Treatment of VF and asystole.
SPO
2 MONITORING. Indications for Use: Pulse oximeter is for use in patient at risk of developing hypoxemia.
Contraindications: None known. EtCO
2 MONITORING. Indications for Use: To detect the level of expired CO2,
used for monitoring breathing efcacy and treatment effectiveness in acute cardiopulmonary care, for example, to
determine if adequate compressions are being performed during CPR or rapidly detect whether endotracheal tube has
been placed successfully. Contraindications: None known. LIFEPAK 20e with or without CodeManagement
Module – ECG MONITORING: ECG obtained by placing either electrodes or paddles on patient; allows for heart’s
electrical activity to be monitored and recorded.
Operating Instructions provide important information to help you operate LIFEPAK 20e and
CodeManagement Module. Become familiar with all terms, warnings, and symbols. GENERAL/MANUAL
DEFIBRILLATION/PADDLE WARNINGS and CAUTIONS: Shock or re hazards • Possible explosion • Possible
patient skin burns • Possible device or paddle damage. • Possible device failure, inability to deliver therapy, ineffective
energy delivery, shutdown, or improper device performance • Possible electrical interference with device performance,
implanted electrical device or other equipment • Safety risk • Failure to detect change in ECG rhythm • Possible
failure to detect out of range condition. AED WARNINGS: Possible misinterpretation of data • Pediatric patient safety
risk. ECG MONITORING WARNING: Possible misinterpretation of ECG data. PEDIATRIC ECG MONITORING
AND THERAPY PROCEDURES: Possible patient skin burns. SYNCHRONIZED CARDIOVERSION WARNING:
Possible lethal arrhythmia. • Possible monitor incompatibility. REMOTE SYNCHRONIZATION: Possible lethal
arrhythmia • Possible monitor incompatibility. CPR METRONOME WARNING: CPR delivered when not needed.
NONINVASIVE PACING WARNINGS: Possible inducement of VF • Possible inability to pace • Possible interruption
of therapy • Possible patient skin burns. SPO
2 WARNINGS AND CAUTION: Shock or burn hazard • Inaccurate
pulse oximeter readings • Skin injury • Possible strangulation • Possible equipment damage. EtCO
2 MONITORING
WARNINGS AND CAUTION: Fire hazard • Possible inaccurate patient assessment or inaccurate CO
2 readings •
Possible strangulation • Infection hazard • Possible equipment damage. CODEMANAGEMENT MODULE BATTERY
WARNING: Possible CO
2 monitoring shutdown. REPLACING/REMOVING ELECTRODES WARNING: Possible cable
damage and ineffective energy delivery or loss of monitoring.
U.S. Federal law restricts this device to sale by or on the order of a physician.
Please consult Operating Instructions at www.physio-control.com or call 800.442.1142 for complete list of indications,
contraindications, warnings, cautions, potential adverse events, safety and effectiveness data, instructions for use and
other important information.
Back to contents
For further information, please contact your
Stryker representative or visit our website at
strykeremergencycare.com
Manufactured by:
Physio-Control, Inc.
11811 Willows Road NE
Redmond, WA, 98052 U.S.A.
Toll free 800 442 1142
strykeremergencycare.com
Stryker European
Operations B.V.
Herikerbergweg 110
1101 CM Amsterdam
Netherlands
Tel +31 (0)43 3620008
Fax +31 (0)43 3632001
Distributed by:
Stryker Canada
2 Medicorum Place
Waterdown, Ontario
L8B 1W2
Canada
Toll free 800 668 8323
Stryker UK Ltd
Stryker House
Hambridge Road
Newbury, Berkshire
RG14 5AW
United Kingdom
Emergency Care
This document is intended solely for the use of healthcare professionals. A healthcare
professional must always rely on his or her own professional clinical judgment
when deciding whether to use a particular product when treating a particular
patient. Stryker does not dispense medical advice and recommends that healthcare
professionals be trained in the use of any particular product before using it.
The information presented is intended to demonstrate Stryker’s product offerings.
A healthcare professional must always refer to operating instructions for complete
directions for use indications, contraindications, warnings, cautions, and potential
adverse events, before using any of Stryker’s products. Products may not be available
in all markets because product availability is subject to the regulatory and/or medical
practices in individual markets. Please contact your representative if you have
questions about the availability of Stryker’s products in your area. Specications
subject to change without notice.
Stryker or its afliated entities own, use, or have applied for the following trademarks
or service marks: CodeManagement Module, CODE-STAT, CODE SUMMARY, EDGE
System, LIFEPAK, QUIK-COMBO, REDI-PAK, Stryker. All other trademarks are
trademarks of their respective owners or holders.
The absence of a product, feature, or service name, or logo from this list does not
constitute a waiver of Stryker’s trademark or other intellectual property rights
concerning that name or logo.
03/2021
GDR 3302004_F
Copyright © 2021 Stryker
References
1. Chan PS, Krumholz HM, Nichol G, Nallamothu BK. “Delayed time to debrillation after
in-hospital cardiac arrest.” NEJM. 2008;358:9–17.
2. Stiell IG, Walker RG, Nesbitt LP, et al. “The BIPHASIC Trial: A randomized comparison of xed
lower versus escalating higher energy levels for debrillation in out-of-hospital cardiac arrest.”
Circulation. 2007;115:1511–1517.
3. Koster RW, Walker RG, Chapman F. “Recurrent ventricular brillation during advanced life
support care of patients with prehospital cardiac arrest.” Resuscitation. 2008;78:252–257.
4. Walsh SJ, McClelland AJ, Owens CG, et al. “Efcacy of distinct energy delivery protocols
comparing two biphasic debrillators for cardiac arrest.” Am J Cardiology. 2004;94:378–380.
Back to contents