2023-2024 Academic Catalog Addendum

ADDENDUM TO
McGovern Medical School
2023-2024 Academic Catalog
Add New Master’s Degree Program:
Master of Science in Anesthesia (MSA)
First Class Enrollment - Fall 2024
PROGRAM DESCRIPTION
The Master of Science in Anesthesia (MSA) is a 28-month, full-time, graduate-level program that requires
100 semester credit hours taken over seven consecutive semesters. This competency-based program that
integrates didactic learning, simulation-based training, and clinical instruction to prepare students for a
career as an anesthesiologist assistant.
The MSA program will educate and train students to manage complex clinical cases as part of the
Anesthesia Care Team. Students will learn standard anesthesia technical skills, how to use an anesthesia
machine and understand its complex functions, how to communicate effectively with patients to provide
safe care and how to manage anesthetic cases. After rigorous academic and clinical training, graduates
will be qualified to provide anesthetic care under the direction of a physician anesthesiologist.
Students will receive didactic instruction encompassing all relevant topics appropriate to the clinical
anesthetist. Students will benefit from learning from various teaching platforms, such as problem-based
learning discussions, flipped classroom sessions, and traditional lectures. Procedural skills and anesthesia
case management will be trained in a simulation lab focusing on both technical and non-technical skills to
prepare students for the rigors of the perioperative environment. Students will complete a minimum of
2000 hours of clinical training, gaining exposure to unique and complex surgical procedures by leading
medical and procedural experts at UTHealth Houston and Memorial Hermann Hospital.
Overall, Anesthesiologist Assistants receive training in basic medical science and clinical practice to utilize
modern technology to monitor and interpret data in all anesthesia care environments. Upon completion
of the program, graduates will be able to:
• Gather and interpret patient information
• Synthesize and present organized evaluations of their findings to physicians
• Interpret data from invasive monitoring, administer anesthetics and controlled
substances under the direction of supervising physician anesthesiologists
• Establish and maintain appropriate airway management and provide ventilator support
• Evaluate and treat life-threatening events according to established life support
protocols such as Basic Life Support (BLS), Advanced Cardiac Life Support (ACLS), and
Pediatric Advanced Life Support (PALS).
Upon program completion, students will meet the requirements to take the National Certification
Examination, administered by the National Commission for the Certification of Anesthesiologist Assistants
(NCCAA). After passing, graduates become Certified Anesthesiologist Assistants.
ADMISSION REQUIREMENTS
The MSA program seeks students who have demonstrated excellence in science and mathematics
during their undergraduate education.
General admission requirements for the MSA program are below:
1. Citizenship: Must be a US citizen or permanent resident
2. Degree: A Bachelor’s Degree from an accredited institution of higher education
3. Prerequisites (All prerequisites must be completed prior to matriculation. Course substitutions
will not be considered.) All prerequisites must be completed at a regionally accredited
institution of higher education in the United States, U.S. territory or Canada:
• One semester of human physiology with laboratory OR one semester of human
anatomy and physiology with laboratory
• Two semesters of biology with laboratory
• Two semesters of general chemistry with laboratory
• One semester of biochemistry
• One semester of organic chemistry with laboratory; a second semester of
organic chemistry with laboratory is recommended
• Two semesters of general physics with laboratory
• One semester of advanced college mathematics including calculus
• One semester of statistics or a second semester of advanced mathematics
• One semester of English
*Human anatomy, human physiology and biochemistry must be taken within 5 years of the
application deadline. All other prerequisites must be taken within 7 years of the deadline.
4. GPA: Minimum of 2.8
5. Standardized Test Scores:
• Medical College Admission Test (MCAT) is the preferred standardized exam for
admission.
o Minimum acceptance score: 494.
• Graduate Record Examinations (GRE) scores will be considered.
o Minimum Verbal Reasoning score: 153
o Quantitative Reasoning score: 156
o Analytical Writing Score: 4.0 or above.
Applicants with a strong application but who have not achieved the minimum standardized test score
will be evaluated by the admissions team on an individual basis. Applicants who have taken the MCAT
or GRE more than once will be evaluated based on the highest score achieved. If an applicant has
taken both exams, they should submit official scores from both exams. Acceptance of an applicant
into the program will be at the final discretion of the admissions committee.
6. Volunteer Work Experience: strongly encouraged.
7. Physical and Technical Requirements: All applicants must have the general abilities required of
anesthesia healthcare providers. This includes:
a. Motor skills – the physical ability to perform the technical and procedural functions
required in patient care, including the ability to perform complex two-handed skills.
b. Communication skills – the ability to effectively communicate with patients, faculty,
staff and peers both in written and oral form.
c. Physical health – the physical capacity to stand for prolonged periods of time in an
operating room and/or clinic, the ability to lift up to ten pounds of equipment
(intravenous fluids, monitors and other equipment necessary to administer a complete
anesthetic).
d. Sensory abilities – the ability to assess a patient utilizing the five senses, including sight,
hearing and touch.
e. Professionalism – must exhibit professional behavior, including honesty, altruism,
respect for others, compassion, empathy, and respect for patient privacy.
A disability does not preclude a student from admission. The UTHealth Houston MSA Program is
committed to providing equal opportunities for qualified students with disabilities in accordance
with state and federal laws and regulations. The intent of the law is to ensure equal access to
individuals with disabilities who are otherwise qualified to meet the essential demands of the
program.
For more information see: UTHealth Houston Handbook of Operating Procedures (HOOP) Policy
101 Disability and Pregnancy Accommodation at
https://www.uth.edu/hoop/policy.htm?id=1448050
8. Related Field Experience: shadowing experience, volunteer work in a healthcare setting(s),
previous health-related employment
• A minimum of eight (8) hours shadowing an anesthesia provider
(Anesthesiologist, Anesthesiologist Assistant, or Certified Registered Nurse
Anesthetist) is required prior to the application deadline.
9. Resume: Standard format
10. Personal Statement: A narrative explaining your motivation for applying to the Master of
Science in Anesthesia Program.
11. Letters of Recommendation: Three professional letters of recommendation from individuals
who can attest to your strengths and weaknesses. Evaluators will upload their letters onto the
CASAA online evaluation portal (see application process). Confidential letters are preferred.
Evaluations should specifically be written to describe the applicant’s potential contribution to
the field of medicine as an anesthesiologist assistant. Receipt of letters of recommendation that
are written for other programs will not qualify.
12. Interview: Includes assessment of communication skills and social engagement, in addition to
motivation/interest to enter the field.
13. Transfer of Credit: The MSA program does not accept transfer of credits from other MSA
programs.
APPLICATION PROCEDURE
Applications should be submitted online to the UTHealth Houston Office of the Registrar
https://www.uth.edu/registrar/applicants/application-forms.htm
The following are required:
a)
A completed application form with a curriculum vitae. Each applicant will be required to submit a
personal statement that explains their interest in becoming an Anesthesiologist Assistant.
b)
Letters of reference (3) on official letterhead from individuals who are qualified to evaluate the
applicant’s academic or professional performance, as well as ability and motivation to complete
the program.
c)
Official transcripts covering all periods of post-secondary enrollment in accredited institutions of
higher education. Applicants should request the institution to send official (original) transcripts
directly to the Office of the Registrar. Graduates of Texas colleges and universities should request
that transcripts be sent in electronic format. Copies of official transcripts sent by the applicant are
not considered. Transcripts must include both grades and credit hours.
d)
Applicants who are nationals of countries where English is not the parent language are required to
submit scores from the Test of English as Foreign Language (TOEFL). See application form for
current requirements and exceptions.
e)
A $60 non-refundable application fee.
Applicants can contact the MSA Program Manager, Kimesha Webb (kimesha.webb@uth.tmc.edu
) for
further questions regarding the application process. The MSA program utilizes a rolling admission system
where early offers can be made. The application must be completed by May 31st, 2024 for admission to
the class matriculating in August of 2024.

Address application
inquiries to:
Office of the Registrar
The University of Texas Health Science Center at Houston
P.O.
Box 20036
Houston, Texas 77225-0036
713-500-3388
Once an application has been submitted, the applicant will receive a PIN number from the Office of the
Registrar. Once the PIN number is received, the status of the application, transcripts, and letters of
reference can be checked online at MyUTH (https://my.uth.tmc.edu)
TUITION AND FEES
Beginning Fall 2024, the MSA resident tuition will be $1,080 per semester credit hour. The non-resident
tuition will be $1,920 per semester credit hour.
Tuition and fees are subject to change and become effective on the date enacted. The Texas Legislature
does not set the specific amount for any particular student fee. Student fees are authorized by state
statute; the specific fee amounts and the determination to increase fees are made by the university
administration and The University of Texas System Board of Regents.
Please refer to the Office of Registrar website at
https://www.uth.edu/registrar/current-
students/registration/tuition-fee-schedule.htm for the current Tuition and Fee Schedules. This site
reflects current information regarding tuition and fee exceptions and/or waivers, Veterans education
benefits, and the Policy for Texas Resident Tuition.
DEGREE REQUIREMENTS
Students are required to complete 100 semester credit hours of coursework and to have participated in a
minimum of 600 total anesthesia cases for completion of the MSA program. Students need to have a
minimum of 2000 clinical hours to satisfy graduation requirements.
Time Limit to Completion:
Students must graduate within no more than four years after matriculation.
CURRICULUM
The curricular progression of the MSA program will provide a sequence of subjects leading to competence
appropriate to the level of study and requirements promulgated by the Commission on Accreditation for
Allied Health Education Programs (CAAHEP). The MSA program will be a contiguous seven-semester
model (including summer sessions) encompassing a combination of didactic and simulation-based
learning as well as significant clinical experience in anesthesia and perioperative medicine. A feature of
the program will be an early introduction into the clinical setting to apply basic science and anesthesia-
specific didactic knowledge. The primary clinical training sites will be at clinical affiliate anesthesiology
groups within the Texas Medical Center located in Houston. Senior and advanced clinical experiences will
also be gained at affiliated facilities through strategic partnerships with community anesthesiology groups
throughout the Houston region and the State of Texas.
The curriculum is divided into three areas: (1) didactic coursework, (2) simulation labs, and (3) clinical
work. Didactic courses are designed to build base knowledge of organ systems and their functions,
pathophysiology, medical terminology, and the utility and function of anesthesia-related equipment.
Simulation experience is utilized to apply didactic knowledge in a safe environment where students can
practice both technical and clinical practice skills. Lastly, students further strengthen their clinical
knowledge by working with physician anesthesiologists and certified anesthesiologist assistants to manage
patients in a clinical setting, focusing on airway management, hemodynamic support, anesthesia
induction, maintenance and extubation, lab interpretation, crisis management and other core skills.
*There will not be an option to transfer credit, receive credit for professional experience or to place out
of courses.
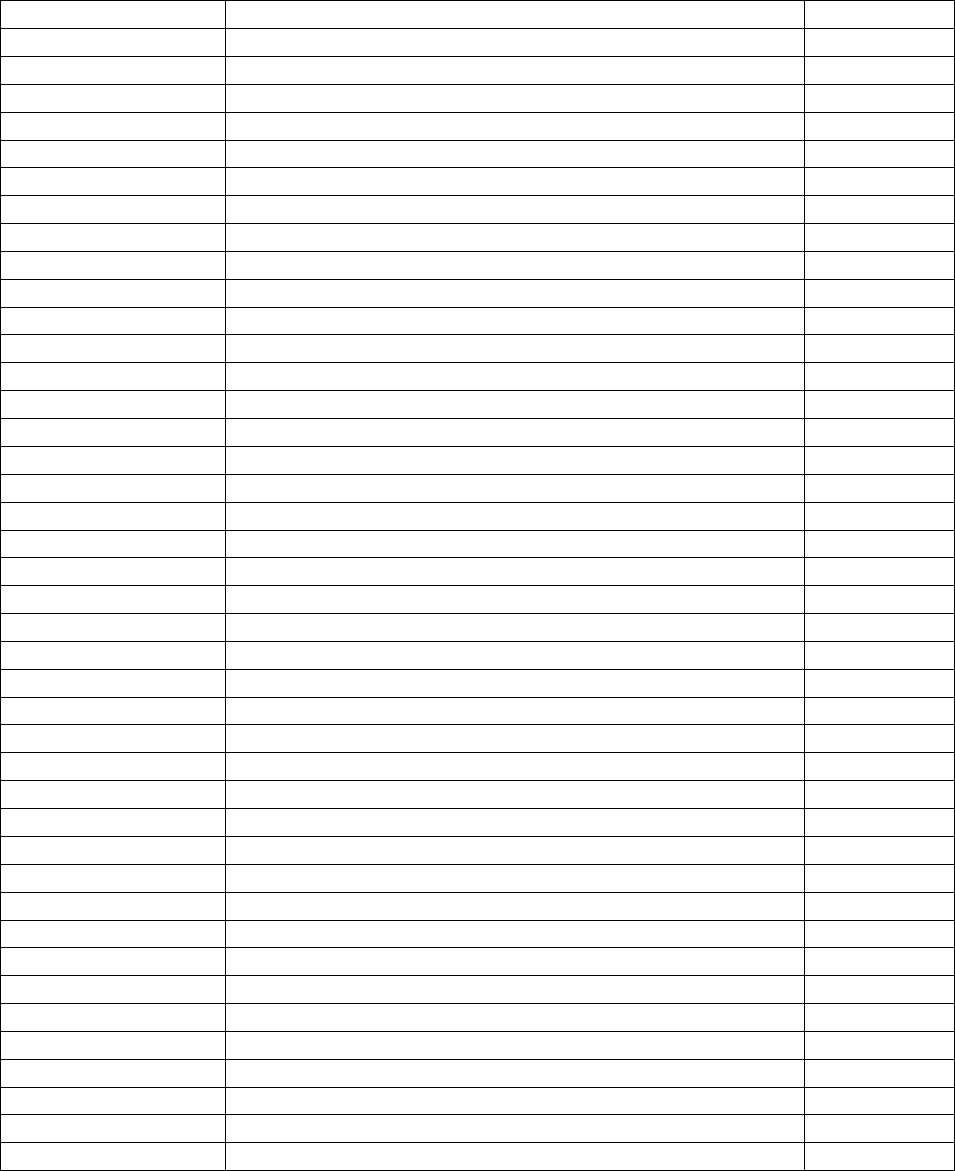
SEMESTER 1-Fall
COURSE NAME
SCH
ANES
Introduction to Physiology I
3
ANES
Anatomy
4
ANES
Pharmacology for the Anesthesiologist Assistant I
2
ANES
Medical Terminology
1
ANES
Airway Management
2
ANES
Introduction to Physiological Simulation
3
ANES
Orientation to Clinical Anesthesia
3
Total
18
SEMESTER 2-Spring
ANES
Patient Monitoring and Instrumentation I
2
ANES
Pharmacology for the Anesthesiologist Assistant II
2
ANES
Applied Physiology in Anesthesia I
3
ANES
Electrocardiophysiology (ECG)
1
ANES
Anesthesia Principles & Practice I
2
ANES
Principles of Life Support
1
ANES
Clinical Anesthesia Experience I
3
ANES
Case Based Simulation I
3
Total
17
SEMESTER 3-Summer
ANES
Anesthesia Principles & Practice II
2
ANES
Applied Physiology in Anesthesia II
3
ANES
Patient Monitoring and Instrumentation II
2
ANES
Clinical Anesthesia Experience II
3
ANES
Case Based Simulation II
2
Total
12
SEMESTER 4-Fall
ANES
Ethics & Professionalism
1
ANES
Anesthesia Principles & Practice III
2
ANES
Applied Physiology III
2
ANES
Current Trends in Anesthesia I
1
ANES
Clinical Anesthesia Experience III
8
ANES
Crisis Management Simulation
1
Total
15
SEMESTER 5-Spring
ANES
Anesthesia Practice Review I
1
ANES
Clinical Anesthesia Experience IV
10
ANES
Subspecialty Case Based Simulation I
1
Total
12
SEMESTER 6-Summer
ANES
Board Preparation
1
ANES
Anesthesia Practice Review II
1
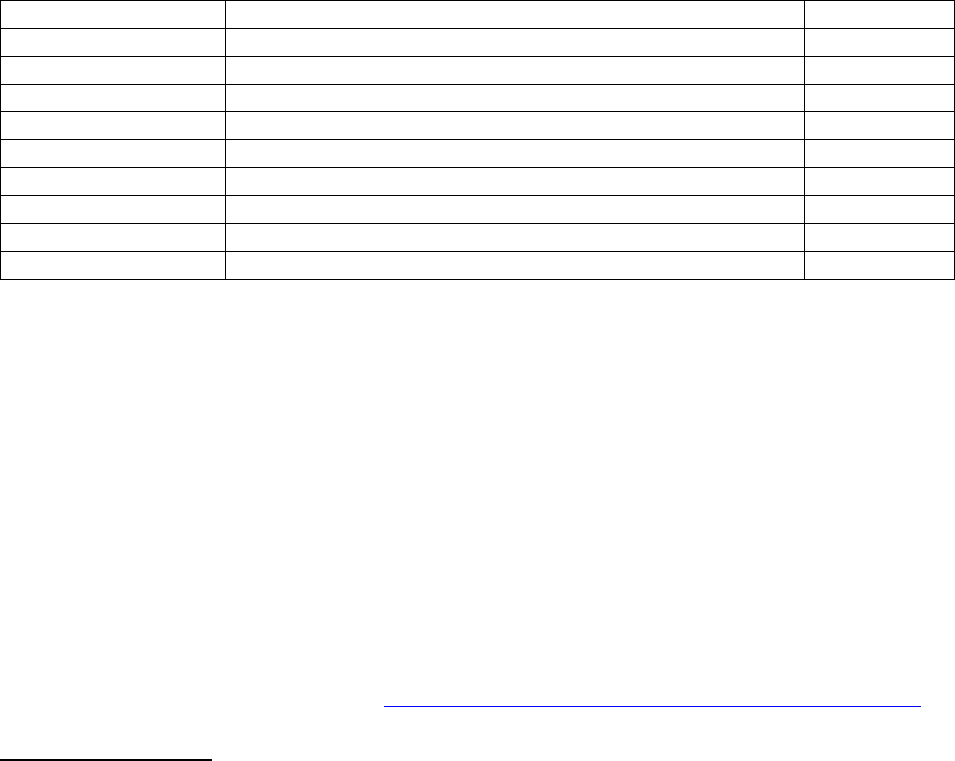
ANES
Clinical Anesthesia Experience V
10
ANES
Subspecialty Case Based Simulation II
1
Total
13
SEMESTER 7-Fall
ANES
Anesthesia Practice Review III
1
ANES
Clinical Anesthesia Experience VI
10
ANES
Subspecialty Case Based Simulation III
1
ANES
Subspecialty Elective
1
Total
13
TOTAL SEMESTER CREDIT HOURS FOR COMPLETION
100
Graduation Requirements:
1. Satisfactory completion of the program of study
2. Satisfactory clinical performance as determined by the Program and Clinical faculty
3. Satisfactory discharge of all financial obligations to the University
4. Received recommendation for being awarded the degree Master of Science in Anesthesia from the
Program Director, Medical Director(s) and approval by the Dean of the McGovern Medical School
at UTHealth Houston.
5. Special program requirements:
a. Participation in a minimum of 2,000 clinical hours of direct patient care
b. Participation in a minimum of 600 anesthetics
c. Meet requirements for application to take the National Certification Examination administered
by the National Commission for the Certification of Anesthesiologist Assistants (NCCAA): Eligibility
to sit for the NCCAA Certification Exam includes graduation from an approved educational
program, along with completion and documentation of NCCAA Standards of Clinical Experience.
More information can be found here: https://www.nccaatest.org/CertificationExamHandbook.pdf
COURSE DESCRIPTIONS
SEMESTER I
ANES Introduction to Physiology I: Students will learn technical skills like peripheral intravenous catheter
placement and participate in simulated clinical scenarios. This course will focus on patient monitoring
(pulse oximetry, capnography, blood pressure measurement, heart rate/EKG, temperature, respiratory
rate), exploration of anesthesia machine functionality, anesthetic alarm interpretation, breathing circuits,
cardiac output monitoring, arterial pressure monitoring and central venous pressure monitoring.
ANES Anatomy: This course will integrate structural anatomy with radiographic visualizations to establish
foundational knowledge necessary to comprehend and explore the anesthetic techniques utilized
clinically to provide anesthesia for a complex array of surgical procedures, especially orthopedic cases
benefiting from regional anesthetic techniques.
ANES Pharmacology for the Anesthesiologist Assistant I: The focus of this course is to instruct students
on the pharmacokinetics and pharmacodynamics of the most commonly used medications in anesthesia.
ANES Medical Terminology: Students will be taught common medical terminology, abbreviations and
symbols used to describe procedures, techniques, imaging types, body systems, disease processes and
procedures.
ANES Airway Management: This course will explore the anatomy, structure, function and management
of both the adult and pediatric airways. Students will be taught how to use standard airway equipment
to secure an airway. Emphasis will be placed on bag-mask ventilation, oral airway placement, nasal airway
placement, laryngeal airway placement, intubation, and confirmation of adequate ventilation. Students
will begin to explore the techniques and methods employed when basic airway skills are unsuccessful in
securing an airway, such as fiberoptic intubation, video-assisted laryngoscopy and surgical airways.
ANES Introduction to Physiological Simulation: Students will learn technical skills like peripheral
intravenous catheter placement and participate in simulated clinical scenarios. This course will focus on
patient monitoring (pulse oximetry, capnography, blood pressure measurement, heart rate/EKG,
temperature, respiratory rate), exploration of anesthesia machine functionality, anesthetic alarm
interpretation, breathing circuits, cardiac output monitoring, arterial pressure monitoring and central
venous pressure monitoring.
ANES Orientation to Clinical Anesthesia: This introductory course will orient students to the clinical
environment and teach them how to assimilate into the anesthesia care team. Topics of study will include:
infection control, universal precautions, hand washing, operating room standard protocols, sterile
technique, an overview of the history of anesthesia, the types of anesthetics delivered, American Society
of Anesthesiologists (ASA) standard monitoring, and the basics of the anesthesia machine.
SEMESTER II
ANES Patient Monitoring and Instrumentation I: This course will explore the ASA standard monitoring
system, advanced patient monitoring, and the associated equipment and technical skills necessary to
monitor patient vital signs. Monitoring modalities taught include electrophysiology, non-invasive and
invasive blood pressure monitoring, bispectral index, pulse oximetry (including the medications and
clinical scenarios that can alter this reading), respiratory gas analysis, temperature monitoring, advanced
hemodynamic monitoring, coagulation studies (TEG analysis), neuromuscular junction monitoring,
transesophageal echocardiography, cerebrovascular testing, microbial analysis and urinalysis.
ANES Pharmacology for the Anesthesiologist Assistant II: This is an advanced course focusing on the
pharmacokinetics and pharmacodynamics of anesthetic agents. Instruction will include topics such as
drug dilutions and calculations, context sensitive half-life and the second gas effect.
ANES Applied Physiology in Anesthesia I: This is an advanced course that will utilize an organ system
approach to teach human pathology. Students will learn how to evaluate the severity of patient disease
to determine anesthetic risk. The major organ systems (cardiac, neurological, renal, gastrointestinal, liver,
and hematologic systems) will be covered.
ANES Electrocardiophysiology (EKG): This course will teach peri-operative electrocardiophysiology
monitoring and advanced cardiac life support. Students will learn how to interpret and monitor EKG
rhythms and manage pathologic conditions that are detected. The course will also emphasize relevant
anatomy, physiology, pharmacology and medical equipment.
ANES Anesthesia Principles & Practice: This course will guide anesthesiologist assistant students on how
to develop the critical thinking skills and advanced technical skills necessary to be a well-rounded,
competent mid-level provider capable of assisting the anesthesiologist and other members of the
perioperative care team manage crisis care. Students will spend a minimum of 40 hours working with the
Department of Anesthesiology Critical Care team, rounding on patients, discussing the appropriate clinical
management of patients with severe burn injuries, sepsis, post-surgical complications, and complex
traumas, amongst many other pathologies.
ANES Principles of Life Support: This course is designed to teach the principles of cardiopulmonary
resuscitation for adults and children. Students will be taught the most up to date resuscitation guidelines
and will become certified in Basic Life Support (BLS) CPR, Advanced Cardiac Life Support (ACLS) and
Pediatric Advanced Life Support (PALS).
ANES Clinical Anesthesia Experience I: This course exposes students to the face-paced, complex
anesthesia intra-operative environment. Students will apply knowledge gained during the introductory
didactic courses to practical clinical cases in the surgical environment. Students will receive supervised
instruction in the operating room one-on-one with a faculty anesthesiologist, resident, certified
anesthesiologist assistant and/or a certified registered nurse anesthetist. This course has a 150-hour
minimum in-hospital time for successful completion.
ANES Case-Based Simulation I: Students will engage in active learning and critical thinking by participation
in clinical case-based scenarios structured to cover the most commonly encountered intra-operative
complications. The cases will develop students’ understanding of applied physiology, pharmacology, and
advanced monitoring skills to detect and remedy simulated patient anesthetic complications and
hemodynamic perturbations.
SEMESTER III
ANES Anesthesia Principles & Practice II (ICU): In this advanced course, students will spend a minimum
of 40 hours working with the Department of Anesthesiology Critical Care team, rounding on patients,
discussing the appropriate clinical management of patients with severe burn injuries, sepsis, post-surgical
complications, and complex traumas, amongst many other pathologies.
ANES Applied Physiology in Anesthesia II: This advanced course will take a more in-depth exploration of
human systemic functions and pathology. This course will take a more in-depth exploration of the human
body’s systemic functions and will focus on how derangements in these systems affect the evaluation of
and ASA classification of patients, specifically how knowledge of patient physiological derangements
affects their overall anesthetic risk for morbidity and mortality. The major organ systems (cardiac,
neurological, renal, gastrointestinal, liver, and hematologic systems) will be covered.
ANES Patient Monitoring and Instrumentation II: This is an advanced course focusing on how to provide
anesthetic care for complex patients. The emphasis is on advanced patient monitoring techniques,
equipment and modalities.
ANES Clinical Anesthesia Experience II: Students will continue to develop the skills and foundations of
clinical practice needed to safely execute an anesthetic plan. Students will actively participant in clinical
cases, honing their intubation, extubation, and peripheral intravenous access placement skills. Students
will also engage in active discussion with the faculty members to review the core principles of
anesthesiology and discuss the relevant clinical pearls of each case they participate in. This course has a
150 hour- minimum in-hospital time for successful completion.
ANES Case-Based Simulation II: This course is a continuation of ANES 115. In the setting of an anesthesia
simulation lab, students will engage in active learning and critical thinking by participating in clinical case-
based scenarios structured to cover advanced anesthesia monitoring, instrumentation, and crisis
management. The cases will develop students’ understanding of applied physiology, pharmacology, and
advanced monitoring skills to detect and remedy simulated patient anesthetic complications and
hemodynamic perturbations.
SEMESTER IV
ANES Ethics and Professionalism: This course will explore the professionalism expectations and
obligations of healthcare personnel with a focus on peri-operative specific concerns such as respect for
patient privacy (HIPPA laws), resolving conflicts, conflict of interest, abuse of authority, sexual
harassment, accountability, integrity, wellness/burnout prevention, substance abuse and mandatory
reporting. The second half of this course will utilize case-based scenarios to explore common ethical
issues that arise in anesthesia. Students will learn the four main principles of bioethics (beneficence, non-
maleficence, respect for patient autonomy, and justice), explore frameworks used to guide ethical analysis
and be educated on which resources are available to assist with resolving ethical dilemmas.
ANES Anesthesia Principles & Practice III: This course will explore the issues that commonly arise in the
post-anesthesia recovery unit (PACU). This is an excellent opportunity for students to observe the issues
that can arise following anesthesia administration and/or post-surgical complications. Emphasis will be
placed on airway management (airway obstruction, hypoventilation, vomiting, aspiration risk,
hypercarbia, hypoxia) concerns, and post-operative hemodynamic monitoring.
ANES Applied Physiology III: This course will take a more in-depth exploration of the human body
systemic functions and will focus on how derangements in these systems affect the evaluation of and ASA
(American Society of Anesthesiology) classification of patients, specifically how knowledge of patient
physiological derangements affects their overall anesthetic risk for morbidity and mortality. The major
organ systems (cardiac, neurological, renal, gastrointestinal, liver, and hematologic systems) will be
covered.
ANES Current Trends in Anesthesiology: This course provides an overview of the most up-to-date
literature, emerging technologies, novel treatment modalities, new mediations, and current research
trends/findings.
ANES Clinical Anesthesia Experience III: In this course, students will begin to rotate on the advanced
anesthesia clinical services such as Pediatric Anesthesia, Cardiovascular Anesthesia, Obstetrical
Anesthesia, Trauma, Neurosurgical Anesthesia, Pediatric Cardiovascular Anesthesiology, and Advanced
Orthopedic Surgical Anesthesia with an Acute Pain Management Focus. Students will receive supervised
instruction in the operating room. This course has a 150 hour- minimum in-hospital time for successful
completion.
ANES Crisis Management Simulation: Students will learn peri-operative crisis management techniques
and skills through in a simulation lab.
SEMESTER V
ANES Anesthesia Practice Review I: This course is designed to prepare students for transition into the
clinical workforce. Content will include reviewing hospital policies, practices, licensure, advocacy, Title IX
requirements, and professionalism guidelines. There will be lectures, required readings and discussions
with faculty and visiting speakers.
ANES Anesthesia Clinical Experience IV: This course provides dedicated clinical time for senior anesthesia
assistant students to hone their clinical, technical, and deductive reasoning skills in the operating room.
Students will work one-on-one with anesthesia faculty and anesthetists to perform pre-operative
evaluations of patients, obtain anesthesia consent for surgery, execute an anesthetic plan, appropriately
monitor patients, manage the airway and place any invasive lines needed for the procedure. Monthly
required readings will be assigned.
ANES Subspecialty Case Based Simulation: Students will explore the management of complex sub-
specialty (Pediatrics, Cardiac, OB, Neuro) cases in a simulated environment.
SEMESTER VI
ANES Board Preparation: This course will review the key content covered in the National Certifying Exam
for the Certification of Anesthesia Assistants.
ANES Anesthesia Practice Review II: This course is designed to prepare students for transition into the
clinical workforce. Content will include reviewing hospital policies, practices, licensure, advocacy, Title IX
requirements, and professionalism guidelines. There will be lectures, required readings and discussions
with faculty and visiting speakers.
ANES Clinical Anesthesia Experience V: This course entails clinical instruction in operating rooms, the
labor and delivery suite and in ambulatory surgery centers. Students will work with anesthesia faculty to
perform pre-operative evaluations of patients, obtain anesthesia consent for surgery, execute an
anesthetic plan, appropriately monitor patients, manage the airway and place any invasive lines needed
for the procedure. Monthly required readings will be assigned.
ANES Subspecialty Case-Based Simulation II: Students will explore the management of complex sub-
specialty (Pediatrics, Cardiac, OB, Neuro) cases in a simulated environment.
SEMESTER VII
ANES Anesthesia Practice Review III: This course is designed to prepare students for transition into the
clinical workforce. Content will include reviewing hospital policies, practices, licensure, advocacy, Title IX
requirements, and professionalism guidelines. There will be lectures, required readings and discussions
with faculty and visiting speakers.
ANES Anesthesia Clinical Experience VI: This is an advanced clinical course that is considered an acting
internship. The focus will be to strengthen technical skills, clinical judgment, and inter-disciplinary team
communication skills.
ANES Subspecialty Case-Based Simulation III: Students will explore the management of complex sub-
specialty (Pediatrics, Cardiac, OB, Neuro) cases in a simulated environment.
ANES Sub-specialty Elective: In this course, the student will complete 80 clinical hours in a sub-specialty
area of interest. This can include Pediatric anesthesia, Obstetrical anesthesia, Trauma, Regional
anesthesia, Cardiovascular anesthesia, Neurosurgical anesthesia, and Non-operative Anesthesia. The
student will devise a project proposal in collaboration with a faculty member of their choosing that
summarizes the clinical pearls of the subspecialty. The student will present the content to their student
colleagues during WAC.
ACADEMIC EXPECTATIONS
The MSA Program is overseen by the McGovern Medical School. All students enrolled at UTHealth
Houston must adhere to UTHealth Houston Handbook of Operating Procedures (HOOP) as well as follow
school policies. Faculty of the MSA program will evaluate students and promote and graduate only those
who have achieved a passing score in all curriculum components. If a student does not meet the
requirements of courses as outlined in the syllabus, they must remediate the course. Students will be
assessed on clinical performance, technical skill progression, professionalism, scholarship, research and
effective communication skills.
Student performance is assessed based on observed performance in inpatient and outpatient facilities,
ambulatory surgery centers, pre-operative anesthesia clinic, the obstetrical suite, the operating arena and
in the classroom.
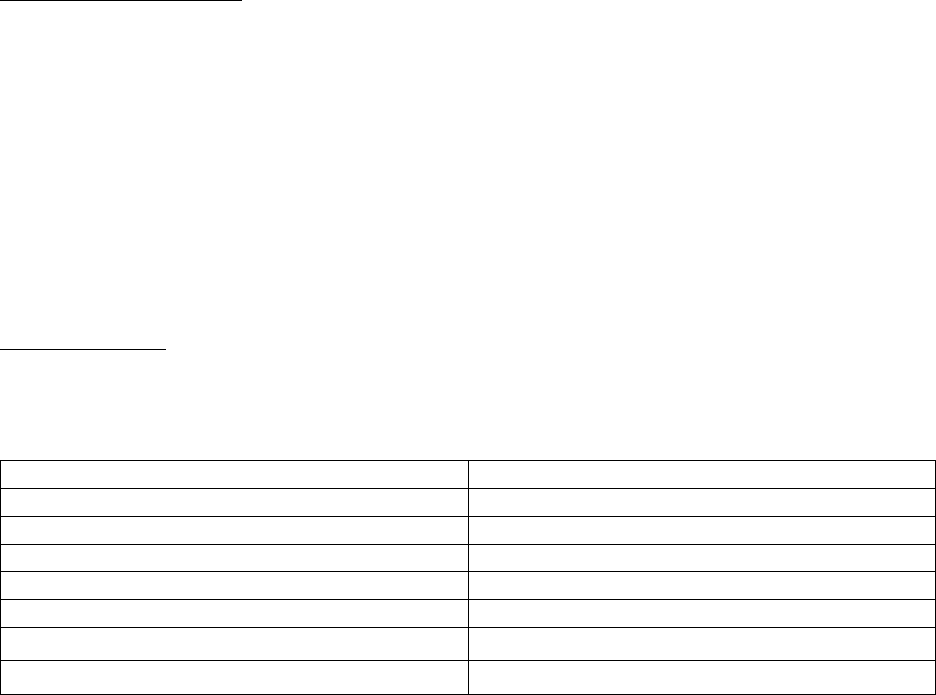
GRADING SYSTEM
Didactics Courses
Didactics courses will follow a traditional letter grade (A, B+, B, C+, C, D, and F) and are calculated into
the GPA.
The corresponding grading scale is as follows:
Letter Grade
Numeric Range
A
90-100
B+
85-89
B
80-84
C+
75-79
C
70-74
D
67-69
F
<67
The grade point average (GPA) is the sum of earned grade points divided by the sum of credit hours passed
and failed. Students receive exam grades following each exam and course grades at the end of each
semester. Students must pass all courses each semester to progress to the next semester.

Clinical Performance:
Clinical rotations will be graded as Pass or Fail.
Clinical performance is assessed based on knowledge of practice, patient care, communication skills,
professionalism, interdisciplinary/inter-professional communication, attendance, case-log
documentation, scholarship (specifically evaluations from journal club and case presentations), and
demonstration of ethical practice.
Case Logs:
All students are required to keep an accurate daily log of clinical activities in the case log system. Students
must enter case information on the same day they participated in the care of the patient. Students will
meet with their faculty advisor each semester to review the cases entered for the semester. A
determination will be made whether the student is on track to meet the minimum case number for
graduation.
The Commission on Accreditation of Allied Health Educational Programs (CAAHEP) who accredits all
anesthesia assistant education programs, requires students to have 600 total anesthesia cases and 2000
total clinical hours for graduation.
Satisfactory academic standing for the MSA program requires that students maintain a minimum grade
point average of 3.0 on a 4-point scale. If a student’s GPA falls below 3.0 at the end of any semester, the
student will not be allowed to continue in the program. To continue in the program, students must petition
the Program Director, who will convene a MSA Progress & Promotions Committee (P&P Committee)
hearing to decide the student’s status in the program. The P&P Committee evaluates the performance of
students with academic difficulty and determines whether remediation or separation is warranted. The
committee will review the student’s cumulative record, faculty evaluations, and reported clinical
performance to determine if the student should progress to promotion, continue remediation or be
dismissed from the program.
The P&P Committee will notify students in writing of any action taken pursuant to this HOOP Policy 220
Student Complaints located at
https://www.uth.edu/hoop/policy.htm?id=2553c1c1-c490-4ad0-a570-
e263e12e0dff
For information regarding the grade grievance procedures at the McGovern Medical School please see:
https://med.uth.edu/admissions/student-affairs/grade-grievance-procedure/
GRADUATION REQUIREMENTS
In addition to other standards set out by this Catalog, graduation from the MSA Program requires that
all of the following are met:
a. Students must maintain a grade point average (GPA) of 2.8 or higher in the first two semesters.
b. Students must finish the program of study in 4 years or less. This is inclusive of leaves of
absence.
c. Students must achieve a minimum GPA of 3.0 to demonstrate mastery of the program content.
d. Students must be found suitable for clinical practice. Suitability for clinical practice is assessed
through overall performance, including didactic course GPA (numerically graded with minimum
passing score for each course determined by each course instructor) and clinical course
performance (graded by evaluations from faculty, comprehensive exams and professionalism
scoring). For more information, please refer to the MSA Student Handbook.
e. Student must have completed degree requirements of 100 semester credit hours and 2000
clinical hours.

PROGRESS AND PROMOTIONS
UTHealth Houston MSA students will be able to view their didactic and clinical performance online
through Canvas. Each MSA student will be assigned a faculty advisor. Students may request a meeting
with their faculty advisor to discuss their progress in the program and any concerns that may arise. Faculty
advisors will monitor each student’s performance throughout the semester and will provide feedback
regarding academic performance, clinical performance and professionalism.
Faculty advisors will schedule a progress and promotions meeting when the student is failing to meet the
expected requirements. The MSA Progress and Promotions Committee is comprised of the Program
Director, the Assistant Program Directors, the Medical Directors, the Program Manager and the core
program didactic faculty. The committee reviews the student’s performance each semester to determine
if the student will be promoted to the next semester. The committee will determine whether students
who are not eligible for promotion may require remedial coursework/performance plans and will
subsequently be re-evaluated for promotion. Students who are required to remediate coursework will
be informed in writing of the specific improvements needed and the expected timeframe during which
they must complete the remediation plan. The committee may also recommend termination from the
program.
At any time, students who self-determine they are unable to perform the expected duties, responsibilities
and/or coursework required to maintain good standing in the UTHealth Houston MSA Program may
voluntarily withdraw from the program.
The MSA Progress and Promotions Committee evaluates overall student performance and makes the final
recommendation on student eligibility for graduation.
ATTENDANCE
To gain the knowledge and skills needed to master the objectives and competencies of the educational
program for the MSA degree, students are expected to maintain consistent participation and attendance
throughout the program. Each course, skills lab, and clinical practicum publishes its required/mandatory
activities; please adhere to those as well as the general absence policy of McGovern Medical School
(MMS). Policies for make-up work are based upon the missed content and are specific to each course. The
McGovern Medical School Absence Policy can be found at https://med.uth.edu/admissions/student-
affairs/policy-excused-absence/
GRIEVANCE POLICY
An academic concern that was not resolved through the informal academic grievance procedures
described above may be addressed through the filing of a formal grievance. Following the unsatisfactory
resolution of an informal grievance, the student may file a formal grievance within seven calendar days of
the failed resolution. The formal grievance must be submitted in writing to the MSA Program Director.
The Program Director will meet with the appropriate parties (students, MSA Course Directors, and MSA
Medical Directors) to seek a resolution that is in the best interest of the individual student, student body,
and the MSA Program as a whole. The Program Director may resolve the issue or invoke a MSA Progress
& Promotions Committee hearing to assist in finding an appropriate resolution. The Program Director will
respond, in writing, within 10 working days of receiving the written complaint. The student will be notified
in writing of the resolution, as will any other pertinent parties. The student has the right to appeal the
decision of the MSA Progress & Promotions Committee or the MSA Program Director, in writing, to the
Dean of the McGovern Medical School within seven calendar days of the failed resolution should they feel
that the resolution does not following university policy or was made with bias. In this case, the Dean will
review the grievance and previous recommended resolutions and decide regarding final resolution of the
matter. The Dean will respond, in writing, within 10 working days of receiving the appeal request. The
student will be notified, in writing, of the resolution, as will any other pertinent parties. The decision of
the Dean is final.
Students are obligated to make every attempt to resolve grievances with the faculty member prior to filing
a formal grievance request. If the student and the faculty cannot resolve the matter, the student should
follow the grievance procedure as outlined above.
Add Student Accommodation Language
ADD as page 40 (prior to McGovern Medical School Departments and Faculty section)
Students with Disabilities and Attendance Requirements
UTHealth Houston students are expected to be present for all classes (whether in-person or online) or
other forms of required class time to include labs, clinical rotations, or other school required meetings.
Students are also responsible for taking quizzes and examinations in a timely manner according to the
schedule for the courses and programs in which they are enrolled. It is the responsibility of each student
to learn and comply with the standards set in each course’s attendance policy, as explained in the
course syllabus. Students should be aware that, when a course policy allows for a specific number of
absences with no penalty, that number typically includes absences for any reason (including those with
documented justification). In courses with such limits, absences beyond the allowed number create a
presumption that the student has not fulfilled the essential educational requirements of the course, and
therefore, will receive a grade reflecting the deficiency.
Attendance is important to the academic success of a student; however, UTHealth Houston understands
that there may be disability-related reasons for missed classes. A student can request an exception to a
faculty member’s attendance policy through the process outlined in HOOP Policy #101 – Disability and
Pregnancy Accommodation https://www.uth.edu/hoop/policy.htm?id=1448050. Determinations
related to disability-related requests will be made on an individual basis based on a review of related
medical documentation and in collaboration with the School’s 504 Coordinator, the Office of University
Relations & Equal Opportunity, the student, and the faculty member responsible for teaching each
impacted course.
The school is not required to grant accommodations that constitute a fundamental alteration of the
program or course. Specifically, the school does not have to modify a requirement, including
attendance, that is essential to the educational purpose or objective of a program or class. Decisions
regarding essential requirements of a course or program will be made by a group of people who are
trained, knowledgeable, and experienced in the area through a careful, thoughtful, and rational review
of the academic program and its requirements. Decision-makers will consider a series of alternatives for
the essential requirements, as well as whether the essential requirement(s) in question can be modified
for a specific student with a disability.
It is important for the student to discuss contingency plans with their faculty before absences occur to
ensure the repercussion of absences are clear and/or to develop a contingency plan. This process is not
intended to allow for unlimited absences and does not alleviate the student of their responsibility to
complete all assignments, quizzes, and examinations, or participate in class or related activities (if
applicable).
For additional information on the disability accommodation process please see HOOP Policy 101 –
Disability and Pregnancy Accommodation https://www.uth.edu/hoop/policy.htm?id=1448050.